Endocrine glands and endocrine system
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
Endocrine glands and Endocrine system
Endocrine glands (Gr., endo = within + krinein = to secrete):
These glands lack ducts and pass secretions into the surrounding blood directly. Therefore they called ductless glands. e.g. – Thyroid, parathyroid, adrenal, pituitary, pineal body and thymus.
Endocrine system:
the work of co-ordination by endocrine system is slowly by secretion of some chemical substances.
Hormones are secreted in blood
Virtually all body cells
Change in metabolic rate
Seconds to hours or days generally long.
Pituitary and pineal gland
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
Pituitary and Pineal Gland
PITUITARY GLAND
It is pink coloured pea-sized gland about 1.3 cm in diameter and weighs only 0.5 g.
It is located in a bony cavity called sella turcica of sphenoid bone and is attached to hypothalamus via infundibulum.
The pituitary gland has two anatomically and functionally separate lobes, the much larger anterior lobe or adenohypophysis and posterior lobe or neurohypophysis.
Adenohypophysis consists of two portions pars distalis and pars intermedia.
The pars distalis produces cluster of hormones whereas pars intermedia secretes only one hormone called melanocyte stimulating hormone (MSH).
However in humans the pars intermedia atrophies and merges with pars distalis during foetal development.
Hormones of Pituitary Gland and their Action on Target Organs
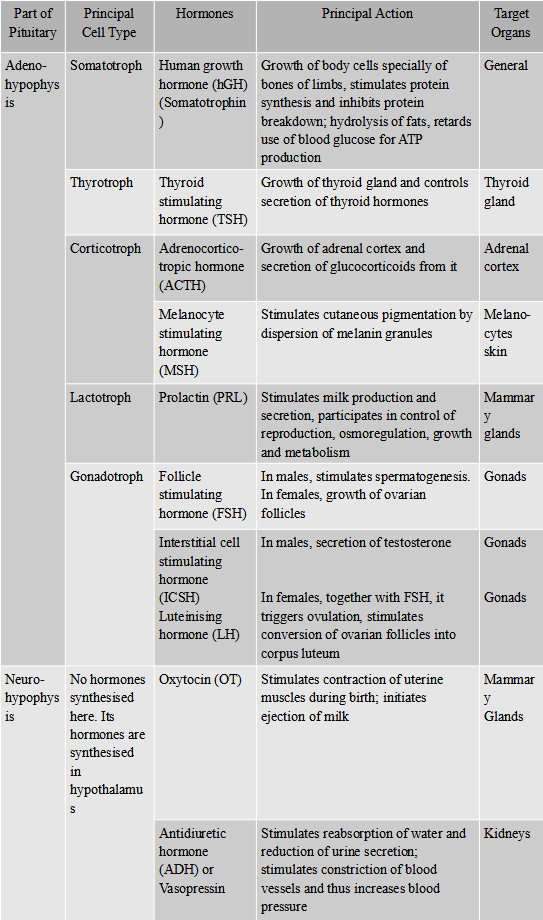
Concept Builder
1. GH is the only adenohyophysis hormone which is linked directly to body whereas other adenohypophysis hormones mostly control other glands.
2. GH stimulates hepatocytes to release glucose into blood. In this respect GH is an insulin antagonist and thus can be related to have diabetogenic effect.
3. Pitocin is synthetic oxytocin which is often given to induce labor.
Pineal Gland
Pineal gland is regarded as vestige of third eye as well as functional endocrine gland.
It is attached to the roof of third ventricle in the rear portion of brain, ectodermal in origin is known as the pineal gland, named for its resemblance to a pine cone.
It has no direct connection with central nervous system.
It is variable in size and weighs about 150 mg, but is richly vascularised and secretes several hormones, including melatonin.
In humans, it has no light-sensitive cells, like lower vertebrates, where pineal is eye-like and responds to light.
Pineal gland functions as a biological clock and a neurosecretory transducer, converting neural information.
More melatonin is produced during darkness.
Its formation is interrupted when light enters the eyes and stimulates the retinal neurons.
They transmit impulses to the hypothalamus, and finally to the pineal gland.
The result is inhibition of melatonin secretion.
In this way, the release of melatonin is governed by the diurnal dark-light cycle.
Melatonin also influences body temperature, metabolism, pigmentation, menstrual cycle and defense capability.
Thyroid gland and Parathyroid gland
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
Thyroid Gland and Parathyroid Gland
THYROID GLAND
It is larget butterfly shaped endocrine organ situated in the neck close to the trachea.
The gland consists of two elongated oval lobes joined by a narrow band called isthmus.
It is a highly vascular organ and contains many spherical or oval sac-like follicles.
Cells lining the thyroid follicle; secrete, two thyroid hormones, thyroxine or tetraiodothyronine (T4) and triiodothyronine (T3).
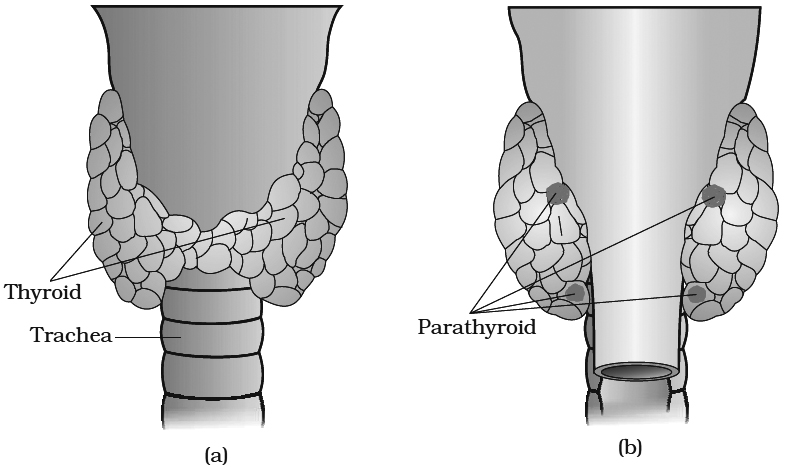
(a) Dorsal side (b) Ventral side
Both are iodinated forms of an amino-acid called tyrosine and remain stored in the jelly like semifluid material (colloid) in the lumen of follicles.
T3 is more active and several times more potent than T4.
From the thyroid mainly T4 is secreted and converted to T3 in peripheral tissues e.g., Liver.
Thyroid is the only endocrine gland which stores its secretory product in large quantity also involve in iodine metabolism.
When necessary, the hormones are released from the colloid to the blood.
In between thyroid follicle are present C-cell or parafollicular cells which release calcitonin (TCT) or parafollicular hormone.
It is involved in calcium homeostasis.
It is hypocalcemic and hypophosphatemic.
Both parathormone and calcitonin help in the maintenance of calcium ions in blood plasma.
Functions:
1.Thyroid hormones greatly increase the metabolic rate of the body and consequently, enhance heat production (Calorigenic effect) and maintains BMR (basal metabolic rate).
2.Thyroid hormones also promote growth of body tissues-both physical growth and development of mental faculties are stimulated.
3.They stimulate tissue differentiation. Because of this action, they promote metamorphosis of tadpoles into adult frogs.
4.To enhance some actions of neurotransmitters : adrenaline and nor-adrenaline.
5.Support process of red blood cells formation.
6.Maintenance of water and electrolyte balance is also influenced by thyroid hormones.
Disorders Due to Thyroid Hormone Imbalances
Hypothyroidism
It can develop due to inactivity of thyroid itself or hyposecretion of TRH or TSH or insufficient dietary intake of iodine.
1.Cretinism:
Failure of thyroid secretion from infancy or childhood slows body and mental development and reduces metabolic rate markedly.
The child remains physically stunted and mentally retarded low intelligence quotient, abnormal skin deaf mutism.
The body temperature, heart rate and blood pressure lower than normal.
The patient is pot-bellied and pigeon chested and has a protruding tongue.
Other features include neonatal jaundice, lethargy, respiratory problems and constipation.
This disease is called cretinism.
Normal growth and development may be restored in certain cases by an early administration of thyroid hormones.
2.Myxedema (Gull's diseases):
Deficiency of thyroid hormones produces myxedema in adults.
The patient has a puffy appearance and lacks alertness, intelligence and initiative.
The patient also suffers from low metabolic rate, slow heart rate, low body temperature and reproductive failure.
Administration of thyroid hormones cures the symptoms. it occurs more commonly in females.
3.Simple Goitre:
In mountainous regions, the dietary deficiency of iodine frequently produces thyroid enlargement (Iodine Deficiency Goitre), accompanied by cretinism or myxedema.
Hyperthyroidism
Exophthalmic Goitre:
In Graye's disease or Exophthalmic goitre, a thyroid enlargement (goitre) is accompanied by a bulging of eyeballs (exophthalmos).
The enlarged thyroid is overactive and secretes excessive amount of thyroid hormones.
So, the goitre is associated with symptoms of thyroid overactivity such as high metabolic rate, rapid heart rate, rise in body temperature, emaciation, nervousness, irritability, tremor and restlessness.
It also occurs more often in females.
It is an autoimmune disorder in which the person produces antibodies that mimic the action of TSH, but are not regulated by normal negative feed back control.
PARATHYROIDS GLAND
These are four small pea sized glands situated very close to the thyroid.
They secrete a hormone called parathormone (Collip's hormone).
They are under the feedback control of blood calcium level.
A fall in blood calcium stimulates them to secrete parathormone, a rise in blood calcium inhibits parathormone secretion from them.
Parathormone increases the concentration of calcium ions in the blood plasma, because it mobilises more calcium from the bones to the plasma and reduces urinary elimination of calcium.
It is secreted whenever the plasma Ca2+ concentration falls and restores the Ca2+ concentration to normal in the plasma.
On the other hand, it increases phosphate elimination in the urine and consequently lower the phosphate concentration in the plasma.
Thus, parathormone regulates the metabolism of calcium and phosphorus.
Calcium Homeostasis:
(i) A higher than normal level of calcium ions (Ca2+) in blood stimulates parafollicular cells of the thyroid gland.
(ii) They release more calcitonin as blood Ca2+ level rises.
(iii) Calcitonin promotes deposition of blood Ca2+ into the matrix of bone tissue. This decreases blood Ca2+ level.
(iv) A lower than normal level of Ca2+ in blood stimulates principal cells of the parathyroid gland.
(v) They release more parathyroid hormone (PTH) as blood Ca2+ level falls.
(vi) PTH promotes release of Ca2+ from bone matrix into the blood and retards loss of Ca2+ in the urine. These actions help raise the blood level of Ca2+.
(vii) PTH also stimulates the kidneys to release another hormone called calcitriol.
(viii) Calcitriol stimulates increased absorption of Ca2+ from foods in the gastrointestinal tract, which helps increase the blood level of Ca2+.
DISORDER OF PARATHYROID
Hypoparathyroidism
Parathyroid Tetany:
If the parathyroids fail to secrete sufficient amount of parathormone, the concentration of calcium ions falls abnormally in the plasma.
This increases the excitability of nerves and muscles due to deficiency of Ca2+ which causes depolarisation without usual stimulus.
Consequently, sustained contractions (tetany) of the muscles of larynx, face, hands and feet are produced.
This disease is called parathyroid tetany.
It can also develop due to accidental damage to the parathyroid or their blood supply during thyroidectomy surgery.
Hyperparathyroidism
The parathyroid tumours secrete excessive amount of parathormone, which causes increased mobilisation of bone minerals into the blood, softening of bones, rise in the concentration of calcium iens in the plasma, and deposition of calcium in kidney tubules and other soft tissues.
It may cause Osteitis Fibrosa Cystica.
Pineal and Thymus gland
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
Thymus and Pineal Gland
Thymus Gland
It is soft bilobed structure where the two lobes lie side by side and joined in the middle by connective tissue.
It is pyramidal in children with maximum size reaching at about 15 years of age.
Its size is reduced somewhat later due to decrease of its lymphoid content.
The weight at birth is 15-20 g in children remaining at that level thereafter.
It is deep red in young age becoming thinner and greyer with age and later yellowing due to infiltration of adipose tissue.
Thymus is covered on the outside by a capsule of loose connective tissue which also penetrates the interior of gland forming septa and irregular lobules.
There is an outer cortex of densely packed thymocytes (or T-lymphocyte lineage) and inner medulla having connective tissue with fewer lymphoid cells.
Balls of flattened epithelial cell called Hassal's corpuscles occur here and there in the medulla.
Thymocytes also occur alongwith some B-lymphocytes.
Hormones produced by the thymus gland is called thymosin.
Thymosin released in the bloodstream has a stimulating effect on the entire immune system.
It promotes proliferation and maturation of T-lymphocytes. It is also called "the throne of immunity", or training school of T-lymphocytes.
Concept Builder
Thymosin play major role in differentiation of T-lymphocytes .which provide cell-mediated immunity. These also promote production of antibodies to provide humoral immunity.
Pineal Gland
Pineal gland is regarded as vestige of third eye as well as functional endocrine gland.
It is attached to the roof of third ventricle in the rear portion of brain, ectodermal in origin is known as the pineal gland, named for its resemblance to a pine cone.
It has no direct connection with central nervous system.
It is variable in size and weighs about 150 mg, but is richly vascularised and secretes several hormones, including melatonin.
In humans, it has no light-sensitive cells, like lower vertebrates, where pineal is eye-like and responds to light.
Pineal gland functions as a biological clock and a neurosecretory transducer, converting neural information.
More melatonin is produced during darkness.
Its formation is interrupted when light enters the eyes and stimulates the retinal neurons.
They transmit impulses to the hypothalamus, and finally to the pineal gland.
The result is inhibition of melatonin secretion.
In this way, the release of melatonin is governed by the diurnal dark-light cycle.
Melatonin also influences body temperature, metabolism, pigmentation, menstrual cycle and defense capability.
Pancreas
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
PANCREAS
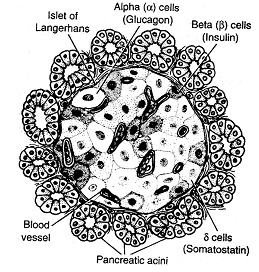
Pancreas and its Hormones:
The pancreas comprises both exocrine and endocrine parts. The endocrine part consists of small masses of hormone secreting cells called ISLETS OF LANGERHANS.

Failure of insulin secretion produces Diabetes mellitus.
In this disease, blood sugar is abnormally high and exceeds the renal threshold for glucose.
Consequently, glucose appears in the urine (glucosuria).
The utilisation of glucose is decreased; instead, catabolism of fats and proteins are enhanced.
Increased oxidation of fat produces ketone bodies such as acetoacetate and acetone.
Also the blood cholesterol rises.
The osmotic effect of glucose in the urine considerably increases the volume of urine (polyuria).
Thirst is enhanced due to urinary loss of water.
Injuries take a long time to heal and may turn into gangrenes.
In extreme cases, the patient suffers from coma and may die.
Administration of insulin reduces the blood sugar and checks other symptoms of diabetes.
Concept Builder
Diabetes Mellitus (Type–I): It is insulin dependent diabetes mellitus (IDDM) and also known as juvenile onset diabetes because it most commonly develops in people younger than 20. It is an autoimmune disorder in which immune system destroys β cells.
Diabetes mellitus (Type–II): It is non insulin dependent diabetes mellitus (NIDDM). It is also known as maturity onset diabetes because it occurs later in life. It arises not from shortage of insulin but because of target cells became less sensitive to insulin.
Testes and ovary
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
Testes and ovary
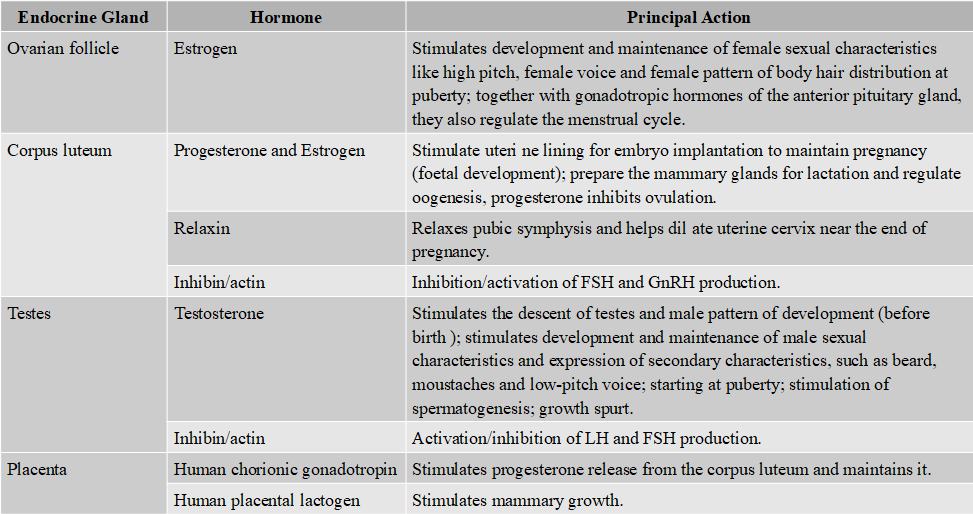
Testes in males and ovaries in females secrete sex hormones at puberty.
Hypogonadism:
Defects in, or injury to, the hypothalamus, the pituitary, or the testes or ovary, result in hypogonadism.
Male hypogonadism can consist of deficient androgen production (hypofucntion of Leydig cell), deficient sperm formation (hypofunction of sertoli cell), or both, before puberty.
It results in the lack of development of secondary sexual characteristics and male musculature.
Female hypogonadism results from hyposecretion of estrogen, resulting in cessation of reproductive cycles.
Such hypogonadism can result from a shortage of pituitary gonadotropins (LH, FSH or both) or can represent primary testicular/ovary failure.
Precocious puberty:
True sexual precocity, i.e., early maturation of ovaries and testes with production of ova before the age of 9 years in girls, or sperm before 10 years in boys, occurs without evident cause.
Sexual pseudoprecocity results from excesses of sex hormones from the adrenal cortex, testis, ovary or from other sources, including extragonadal tumours.
Sexual pseudoprecocity in boys occurs as a consequence of excess of testosterone produced by tumours of the testis or adrenals.
In such cases, enlargement of the penis, accelerated appearance of sexual characteristics, such as, pubic and axillary hair, masculinisation, faster body growth, and ultimate stunting are present.
Sexual pseudoprecocity in girls arises from increased supply of estrogen secreted by tumours of the ovaries or adrenals.
The external manifestations of sexual maturation, for example, breast formation and appearance of pubic hair, appear early, but the maturation and discharge of ova do not occur.
Hormones Regulating Reproduction
Eunuchoidism:
This results from the failure of testosterone secretion.
For this disorder, secondary sex organs, such as prostate gland, seminal vesicles and penis, remains infantile and small in size and fail to function.
Spermatozoa fail to be produced.
External sex characters like beards, moustaches and low-pitch male voice fail to develop.
Gynaecomastia:
It is the development of breast tissue in males, and is usually due to perturbation of estrogen to androgen ratio.
In the neonatal period and during puberty, gynaecomastia is due to temporary increase in circulating estrogen.
Decreased testosterone in later life may also lead to gynaecomastia.
Removal of testes in male is called castration.
It will lead to decline in the androgen level and secondary characters fail to appear.
It can lead to retention of high pitch juvenile voice in a male.
Hormones of heart, kidney and gastrointestinal tract
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
Hormones of heart, kidney and gastrointestinal tract
In addition to endocrine glands, hormones are also secreted by some tissues which are not endocrine glands.
For example, the atrial wall of heart secretes a very important peptide honnone called atrial natriuretic factor (ANF) which decrease blood pressure.
When blood pressure is increased, ANF is secreted which causes dilation of blood vessels.
This reduces the blood pressure.
Juxta glomerular cells of kidney produces peptide hormone called erythropoietin which stimulates erythropoiesis. (Formation of RBC).
Endocrine cells present in different part of the gastro intestinal tract secrete four major peptide hormones namely gastrin, secretin, cholecystokinin (CCK) and gastric inhibitory peptide (mentioned in animal nutrition).
Mechanism of hormone action
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
Mechanism of Hormone Action
Catecholamines, peptide and protein hormones are not lipid-soluble, and so, cannot enter their target cells through the bilipid layer of plasma membrane.
Instead, these water soluble hormones interact with a surface receptor, usually a glycoprotein, and thus, initiate a chain of events within it.
The hormone insulin provides a well-studied example.
Extracellular Receptor:
The membrane bound receptors of insulin is a heterotetrameric protein consisting of four subunits, two a-subunits protrude out from surface of the cell and bind insulin, and two b-sub-unit that span the membrane and protrude into the cytoplasm.
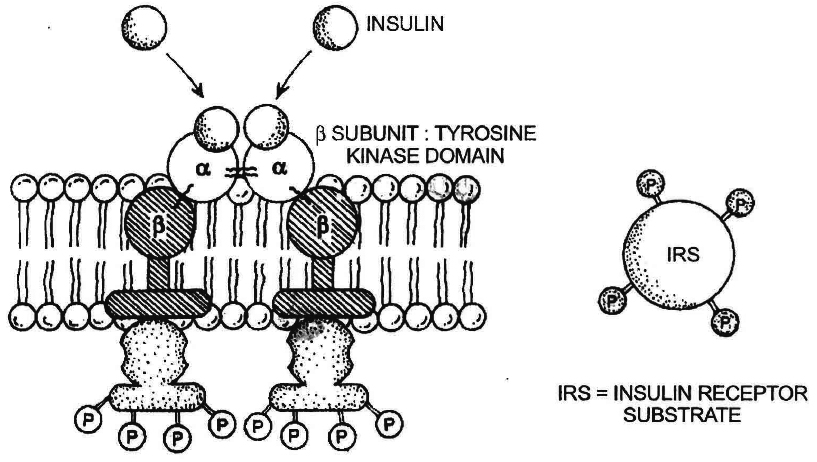
Binding to the receptor:
Binding of insulin to the outer subunits of the receptor causes a conformational change in the membrane spanning b-subunits, which is also an enzyme, a tyrosine kinase.
The activated b-subunits add phosphate groups of specific tyrosine residues located in cytoplasmic domain of the receptor as well as a variety of insulin receptor substrates.
Second messengers-the mediator:
As a result of b-subunit activity, a transducer G-protein activates enzyme phosphodiesterase.
This enzyme breaks phosphatidylinositol 4,5-biphosphate (PIP2) into a pair of mediators: inositoltriphosphate (IP3) and diacylglycerol (DG).
In turn, IP3, which is water-soluble, and so diffuses into cytoplasm and triggers the release of another messenger Ca2+ ions for intracellular calciummediated processes.
While DG remains within the membrane where it activates an enzyme called protein kinase C, which in turn, activates many other enzymes, such as pyruvate dehydrogenase, and so brings about the physiological effects.
Antagonistic effect:
Many cells use more than one second messenger.
In heart cells, cAMP serves as a second messenger, speeding up muscle cell contraction in response to adrenaline, while cyclic guanosine monophosphate (cGMP) serves as another second messenger, slowing muscle contraction in response to acetylcholine.
It is in this way that the sympathetic and parasympathetic nervous systems achieve antagonistic effect on heartbeat.
Another example of antagonistic effect is insulin, which lowers blood sugar level, and glucagon, which raises it.
Synergistic effect:
Another type of hormonal interaction is known as synergistic effect.
Here, two or more hormones complement each other's actions and both are needed for full expression of the hormone effects.
For example, the production, secretion and ejection of milk by mammary gland require the synergistic effect of estrogens, progesterone, prolactin and oxytocin.
Intracellular Receptors:
Unlikely catecholamine and peptide hormones, steroid and thyroid hormones are lipid-soluble hormones and readily pass through the plasma membrane of a target cell into the cytoplasm.
There they bind to specific intracellular receptor proteins, forming a complex that enters the nucleus and bind to specific regulatory sites on chromosomes.
The binding alters the pattern of gene expression, initiating the transcription of some genes (DNA), while repressing the transcription of others.
This results in the production of specific mRNA translation products, proteins and usually enzymes.
The actions of lipid-soluble hormones are slower and last longer than the actions of water-soluble hormones.
These cause physiological responses that are characteristic of the steroid hormones.
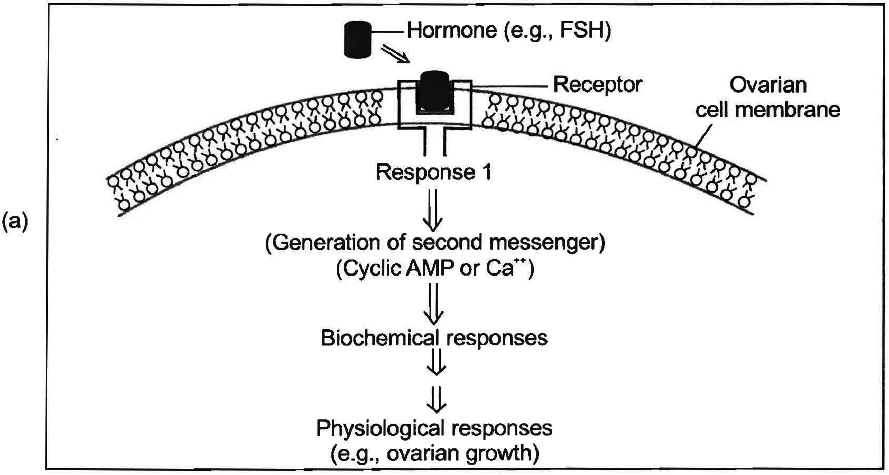
(a) Protein hormone
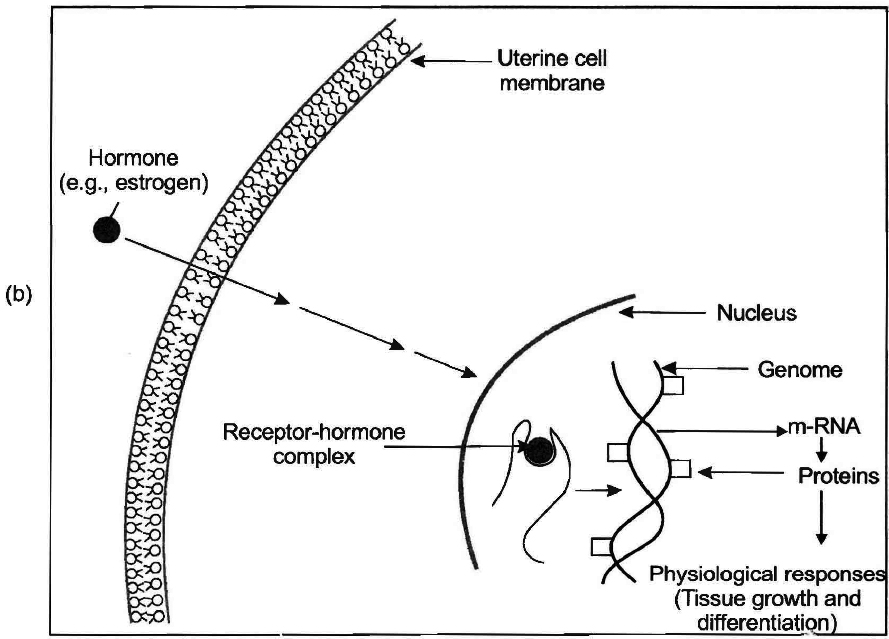
(b) Steroid hormone
 ACME SMART PUBLICATION
ACME SMART PUBLICATION
