Respiratory Organs
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
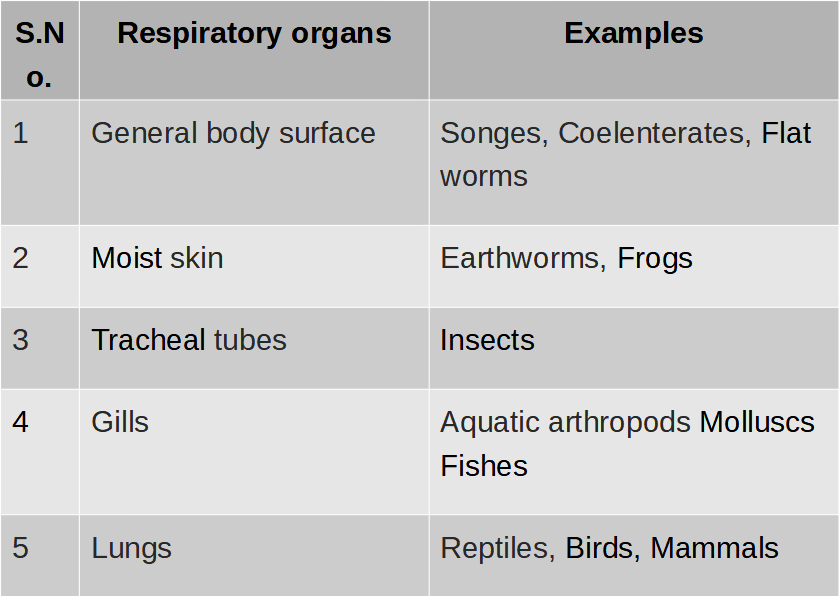
Respiration organs
The process of exchange of O2 from the atmosphere with CO2 produced by the cells is called breathing, commonly known as respiration.
Human Respiratory System
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
HUMAN RESPIRATORY SYSTEM
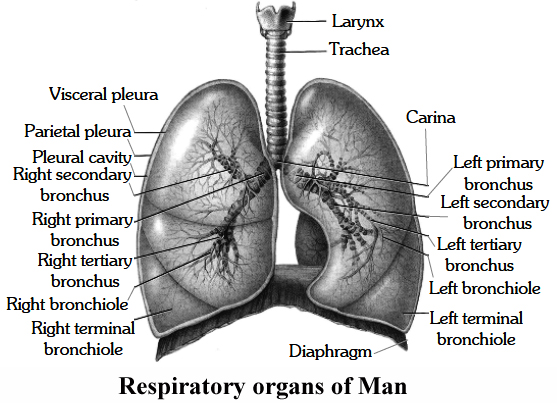
The respiratory system of man consists of the following organs :
1. Nasal Cavity:
The nasal cavity is the first part of the respiratory system.
It opens to the exterior through nostrils.
Nasal cavity is divided into nasal chambers by the nasal septum. Each nasal chamber can be differentiated into three regions.
(i) Vestibular: First part starting from nostril, has oil glands and hair to prevent entry of large dust particles.
(ii) Respiratory part: Highly vascular and involved in conditioning of air as the air gets warmed and moist. Arising from the wall of each nasal chamber, there are 3 shallow bony ridges called nasal conchae. These are individually named as superior, middle and inferior. (Superior lies within the olfactory part; middle and inferior lie in the respiratory part). The conchae are covered with mucus membrane and greatly increase the surface of the nasal chambers.
(iii) Olfactory part: It is the upper part, lined by olfactory epithelium for smell.
2. Pharynx:
From the nasal cavity, the air enters the pharynx.
It serves as a common passage for both air and food.
The opening into the wind pipe or trachea is a narrow slit the glottis.The glottis is protected against the entrance of food by a triangular flap of tissue, the epiglottis.
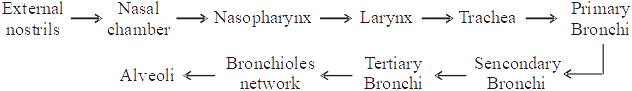
3. Human Larynx:
Until puberty, there is little difference in the size of the larynx ('voice box') in male and female.
The larynx opens into the or opharynx by a slit like aperture, the glottis.
The larynx is composed of irregularly shaped cartilages attached to each other by ligaments and membranes.
The main cartilages are-
(i) Thyroid cartilage is the most prominent, C-shaped, incomplete dorsally, called Adam's apple as it is apple shaped and more prominent in male.
(ii) Cricoid cartilage lies below the thyroid cartila'ge, and its shape is like a signet ring.
(iii) Arytenoid cartilages are two roughly pyramid shaped cartilages forming posterior wall of the larynx.
(iv) Corniculate - These are two conical nodules of elastic fibro-cartilage which lie at the apices of arytenoid cartilages,
(v) Cuneiform - These are two small, elongated, club shaped nodules of elastic fibro-cartilage which lie above and anterior to corniculate cartilages. These connect epiglottis to arytenoid cartilage.
(vi) Epiglottis is a single leaf shaped cartilage which projects into the pharynx,
Thus a total of 9 cartilages -3 paired (iii, iv, v) and 3 unpaired (i, ii, vi).
The thyrohyoid membrane is a broad, flat membrane attached to the hyoid bone above and to the thyroid cartilage below.
Inside the larynx are present two pairs of vocal cords, one pair of false vocal cords which have little to do with sound production and the second inner pair or true vocal cords.
When air is forced through the larynx, it causes vibration of the true vocal cords and sound is produced.
The pitch of a sound is determined by the tension on the vocal cords-the greater the tension, the higher the pitch.
4. Trachea:
The trachea is a tube about 12 cm long with C shaped (dorsally incomplete) rings of hyaline cartilage in its walls.
These rings of cartilage make the wall non-collapsible.
It is internally lined by pseudostratified ciliated columnar epithelium.
Cilia beat to push out the mucus.
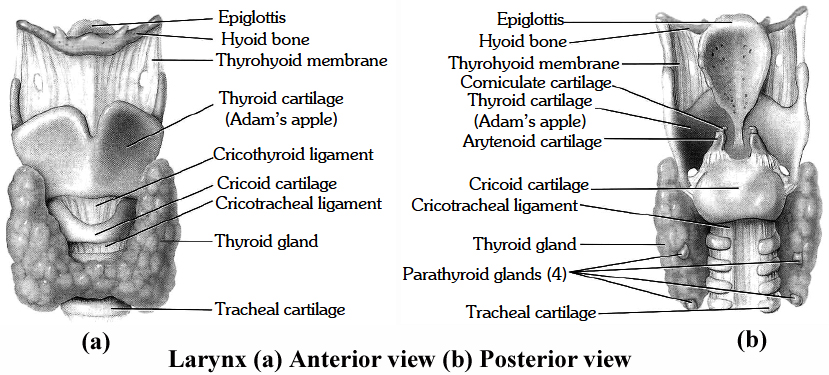
5. Bronchi:
The walls of the bronchi are likewise supported by cartilaginous rings.
Each bronohus divides and redivides into smaller and smaller bronchioles.
Epithelium gradually changes from pseudostratified ciliated columnar epithelium in the bronchi to ciliated simple cuboidal epithelium in the terminal bronchiole.
Incomplete rings of cartilage are gradually replaced by plates of cartilage that finally disappear in a distal bronchiole.
Terminal bronchiole is further subdivided into respiratory bronchioles. Respiratory bronchioles open into alveolar ducts ® atria ® alveolar sacs ® alveoli. From respiratory bronchioles onward the wall is very thin and is made up of simple squamous epithelium.
6. Lungs:
The lungs occupy the greater part of the thoracic cavity.
Surrounding each lung is a double walled sac within the walls of which lies, the pleural cavity.
The right lung is divided into three lobes and left into two.
Inside the lung each bronchus divides into numerous bronchioles, each of which terminates into an elongated saccule, the alveolar duct, which bears on its surface air sacs or alveoli.
The number of alveoli in the human lungs has been estimated to be approximately Respiratory organs of man 300 million.
The lungs are covered by a thin double layer of simple squamous epithelium called the pleura.
The outer or parietal pleuron remains attached to the wall of thoracic cavity.
The space between the two pleural membranes contains pleural fluid for reducing friction and makes the movement of lung easy.
Inflammation of the pleura causes a disease called 'pleurisy'.
Lungs are pink at birth.
They become dark grey and mottled in adults due to deposition of carbonaceous materials.
Darkening increases in smokers and persons exposed to pollutants.
The right lung is shorter by about 2.5 cm due to raised position of diaphragm on the right side to accomodate liver.
The left lung is longer. It is, however, narrower than the right lung because it contains a cardiac notch for accomodating asymmetrically placed heart. Left lung is divisible by an oblique fissure into two lobes, left superior and left inferior.
Right lung has two fissures, horizontal and oblique. They divide the right lung into 3 lobes -right superior, right middle and right inferior. The lobes are divided internally into segments and segments into lobules.
There are 8 segments in the left lung and 10 segments in the right lung. On the average an adult right lung weighs 625 g, while the left lung weighs 565 g.
Mechanism of Breathing
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
MECHANISM OF BREATHING
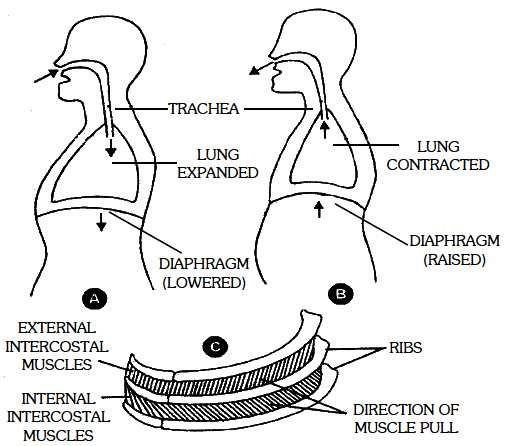
Respiratory movements in man are carried out with the help of intercostal muscles and diaphragm.
There are two phases of each breathing movement, inspiration and expiration.
Mechanism of breathing showing: (a) inspiration, (b) expiration
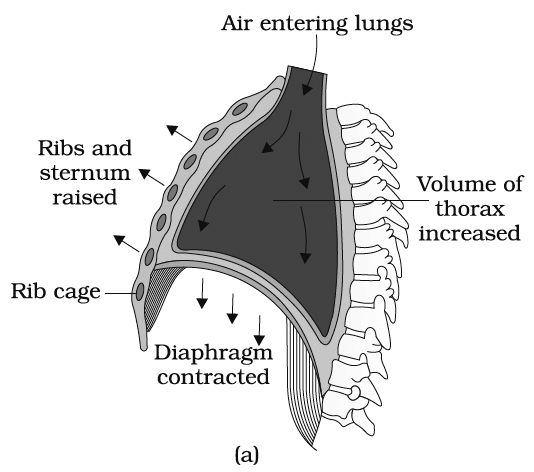
(1) Inspiration (Inhalation).
It involves intake of fresh air in the alveoli of the lungs. It includes an active process and consumes the mechanical energy.
There are two types of inspiratory muscles:
(a) Phrenic muscles: These muscles extend from diaphragm to ribs and vertebral column.
(b) External intercostal muscles. These are 11 pairs of muscles present between 12 pairs of ribs dorsoventrally and laterally. When phrenic muscles contract, the diaphragm is flattened whereas when extemal intercostal muscles contract, the ribs are pulled forward, upward and outward. The thoracic cavity increases in all directions which results in increase in volume and decrease in pressure. So, air moves into the lungs.
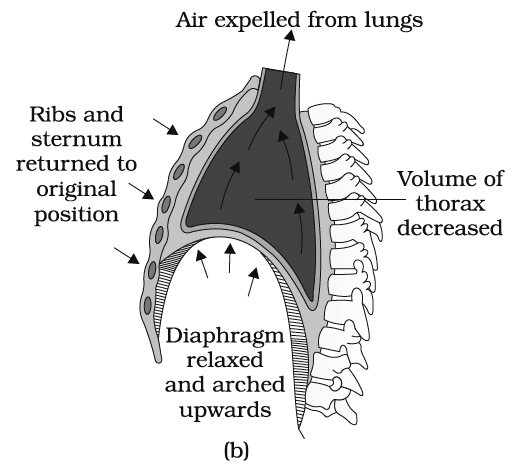
(B) during expiration, (C) at rest
(2) Expiration.
It involves the expelling of air of high pCO2 out of the body.
During rest, the expiration is a passive process and simply involves the relaxation of the inspiratory muscles (phrenic and external intercostal muscles).
These decrease the volume of thoracic cavity. But during forceful expiration, two expiratory muscles also help in expiration:
(a) Abdominal muscles. These extend from the ribs to the abdominal organs. When these contract, the abdominal visceral organs are pulled upward towards the diaphragm. So the diaphragm becomes more convex and thoracic cavity decreases anteroposteriorly.
(b) Internal intercostal muscles. These are also 11 pairs of muscles present between the ribs. When these contract, ribs are pulled backward, downward and inward, so thoracic cavity decreases dorsoventrally and laterally. Due to the above changes larger amount of air is passed out.
Pulmonary Volumes
(i) Tidal volume (TV): The volume of air inspired or expired involuntarily in each normal breath. It is about 500 ml of air in average young adult man.
(ii) Inspiratory reserve volume (IRV) : The maximum volume of air which a person can inhale over and above tidal volume by deepest possible voluntary inspiration. It is about 2500-3000 ml.
(iii) Expiratory reserve volume (ERV) : The volume of air which can be expired over and above the tidal volume with maximum effort. It is about 1000-1100 ml (according to NCERT).
(iv) Residual volume (RV) : The volume of air left in the lungs even after maximum forceful expiration. It is about 1100-1200 ml (according to NCERT).
Pulmonary Capacities
The combination of two or more pulmonary volumes. These include:
(i) Inspiratory capacity (IC) : Tidal volume + Inspiratory reserve volume. It is about 3000 -3500 ml.
(ii) Functional Residual Capacity (FRC) : Expiratory reserve volume + Residual volume. It is about 2500 ml.
(iii) Vital capacity (VC) : Inspiratory reserve volume + Tidal volume + Expiratory reserve volume. It varies from 3500 ml to 4500 ml depending upon age, sex and height of person.
(iv) Total lung capacity (TLC) : It is tidal volume + inspiratory reserve volume + Residual volume + Expiratory reserve volume. It is about 5800 ml.
With the exception of FRC and RV and TLC, all other lung values and lung capacities can be measured with the help of a simple spirometer.
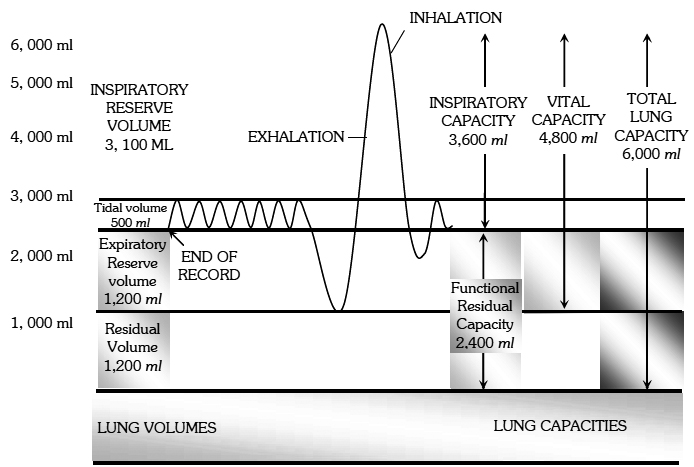
Various pulmonary air volumes
All pulmonary volumes and capacities are about 20% to 25% less in women than in men, more in athletic people than asthmatics.
Exchange of Gases
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
Exchange of Gases
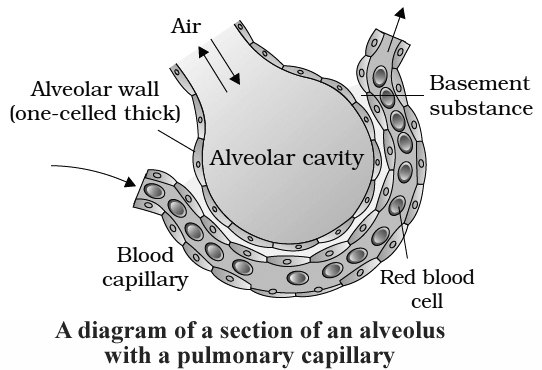
Alveoli are the primary sites of exchange of gases.
Exchange of gases also occur between blood and tissues.
O2 and CO2 are exchanged in these sites by simple diffusion mainly based on pressure/ concentration gradient.
Solubility of the gases as well as the thickness of the membranes involved in diffusion are also some important factors that can affect the rate of diffusion.
Inspired air in the alveoli remains in close contact with blood.
The partition between the two include.
1. Alveolar epithelium
2. Alveolar epithelial basement membrane
3. Thin interstitial space
4. Capillary basement membrane
5. Capillary endothelial membrane
This whole part is called respiratory membrane and cumulatively form a membrane of 0.5 mm thickness.
The limit of exchange between alveoli and pulmonary blood is diffusing capacity.
It is defined as volume of gas that diffuses through respiratory membrane in one minute for a
particle pressure difference of 1 mm Hg.
Solubility of the gases in lipids also affects diffusing capacity.
Diffusing capacity of CO2 is 20 times more than that of oxygen and the diffusing capacity of O2 is about double than that of nitrogen.
Surfactant:
A surface active agent -lecithin secreted by type II alveolar epithelial cells, reduces surface tension between the alveolar fluid and air.
It prevents collapsing of lung alveoli.
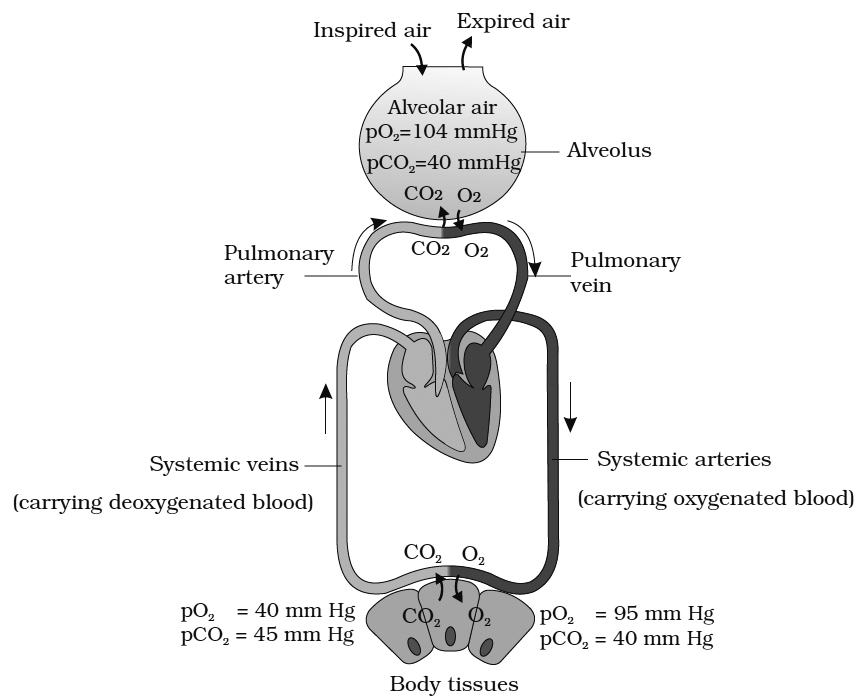
The exchange of gases between the alveoli and blood in the lungs, and the blood and the tissues is the result of difference in partial pressure of the respiratory gases, that is, oxygen and carbon dioxide.
External Respiration or Exchange at Alveoli Level
Partial pressure of O2 in the atmospheric air is 159 mm of Hg and that of CO2 is 0.3 mm of Hg.
Partial pressure of oxygen pO2 in alveolar air is 104 mm Hg and it is only 40 mm Hg in the arterial capillaries of the lungs.
Therefore, oxygen from the alveolar air rapidly diffuses into the blood capillaries due to its higher pO2.
In the expired air, it changes to 116 mm of Hg.
Similarly the pCO2 in the blood reaching the alveolar capillaries is 45 mm Hg whereas pCO2 in alveolar air is 40 mm Hg.
Therefore, CO2 rapidly leaves the blood capillaries and reaches the alveoli.
The pCO2 level in expired air is 32 mm Hg.
Internal Respiration or Exchange at Tissues Level
The gaseous exchange between the blood and body tissues is also due to the differential partial pressures. The pO2 and pCO2 of the arterial blood reaching the tissues is 95 mm Hg and 40 mm Hg respectively. The pO2 and pCO2 of tissues is 20 mm Hg and 52 mm Hg respectively. Therefore, oxygen quickly leaves the blood and enters the cells whereas CO2 produced in the tissues leaves the cells and enters the blood.
FACTORS THAT DECREASE OXYGENATION
1. Low blood volume
2. Anaemia
3. Low Hb
4. Poor blood flow
5. Pulmonary diseases
Transport of Gases
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
Transport of Gases
Oxygen Transport
Each decilitre of blood carries 19.8 ml of 02 of which 5 ml diffuses into tissues.
3% is transported dissolved in plasma and 97% is carried by the RBCs. Four Fe2+ ions of each haemoglobin can bind with 4 molecules of O2 and it is carried as oxyhaemoglobin.
Oxyhaemoglobin dissociates near tissues due to increase in acidity and decrease in pH. It can also be caused due to high temperature.
In a normal person, the haemoglobin level is about 15 per 100 ml.
The capacity of 1 g of haemoglobin to combine with O2 is 1.34 ml.
Therefore, arterial blood carries about 20 ml of O2/100 ml of blood.
Under normal condition, the O2 level falls to about 14.4 ml/100 ml in the venules.
It indicates that under normal condition, approximately 5 ml oxygen is transported by blood.
Under strenous conditions or during exercise, the O2 level falls to about 4.4 ml/100 ml i.e., approximately 15 ml of O2 is transported by Hb during exercise.
Bohr's Effect:
The relationship between the pO2 and percent saturation of haemoglobin when represented on a graph is termed as oxygen-haemoglobin dissociation curve and is sigmoid in shape. A rise in pCO2 or fall in pH decreases oxygen affinity of haemoglobin, raising the P50 value. This is called Bohr's effect (P50 value is the value of pO2 at which haemoglobin is 50% saturated with oxygen to form oxyhaemoglobin). Conversely a fall in pCO2 and rise in pH increases oxygen affinity of haemoglobin and shifts the curve to left. Foetal haemoglobin has a higher affinity for O2 because it binds BPG less strongly. Therefore, oxygen haemoglobin dissociation curve for foetal haemoglobin will appear on the left side.
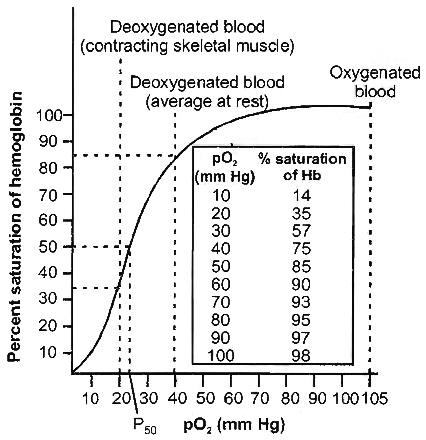
temperature showing the relationship between haemoglobin saturation and pO2
Myoglobin present in the muscles also has more affinity for O2. But since it has only one Fe2+ group, the curve obtained will be hyperbolic, not sigmoid.
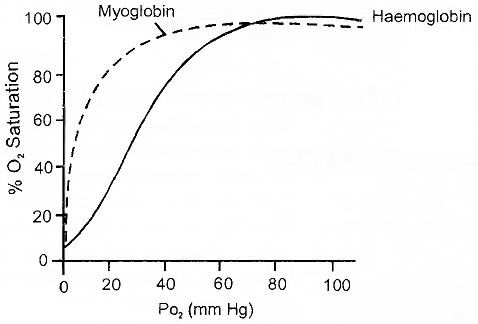
Dissociation curve for haemoglobin and myoglobin at 37°C, pCO2 40 mmHg and pH 7.
Concept Builder
1. Carbon Monoxide Poisoning:
If a person sleeps in a closed room with a lamp burning the absence of sufficient amount of oxygen causes an incomplete combustion of carbon and produces carbon monoxide in the room.
As the person inhales carbon monoxide, it diffuses from the alveolar air to the blood and binds to haemoglobin forming carboxyhaemoglobin.
The later is a relatively stable compound and cannot bind with oxygen.
So, the amount of haemoglobin available for oxygen transport is reduced.
The resulting deficiency of oxygen causes headache, dizziness, nausea and even death.
Carbon monoxide combines with haemoglobin at the same point on haemoglobin molecule as does oxygen.
It binds with haemoglobin 250 times faster than oxygen.
2. SARS (Severe Acute Respiratory Syndrome):
The first patient of SARS was reported on February 26, 2003 in China.
The causative agent is human Corona virus.
It is a new member of influenza virus family which is considered as a mutant form of influenza virus.
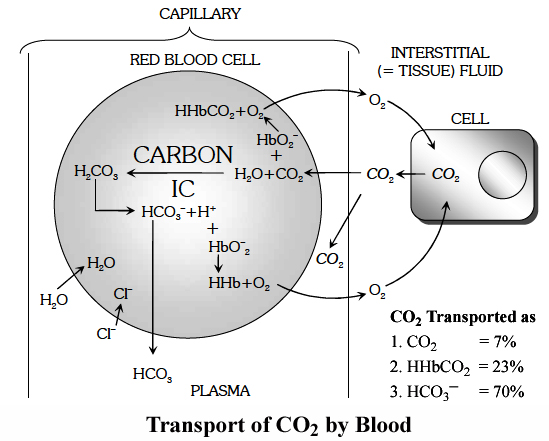
Carbon Dioxide Transport
CO2 is transported in three ways :
1. In dissolved State: About 7% of CO2 is transported after getting dissolved in plasma. The pCO2 in the arterial blood is 40 mm of Hg and in the venous blood, it is 45 mm of Hg. About 0.3 ml of extra CO2 is carried per 100 ml of blood in this form.
2. As Bicarbonate: Nearly 70% of CO2 is transported from tissues to lungs in this form. CO2 diffuses from tissues into the blood and enters RBCs. It combines with water to form H2CO3 which dissociates into H+ and HCO3–. Being catalysed by carbonic anhydrase, it is a very fast step.
![]()
H+ combine with hemoglobin replacing its association with K+ and form hemoglobinic acid.
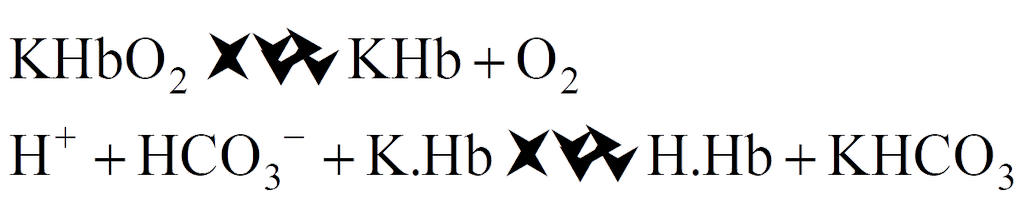
Due to it, the level of HCO3– increases in RBCs, which start coming out of it along the concentration gradient. To maintain ionic balance, Cl– move in from plasma into RBCs.
In the plasma HCO3– combine with Na+ or K+ to form NaHCO3 or KHCO3.
3. As Carbamino-Hb : About 20-25% of CO2 is transported in this mode. CO2 combines with NH2 group of Hb and forms carbamino-Hb. This combination of CO2 and Hb is a reversible reaction.
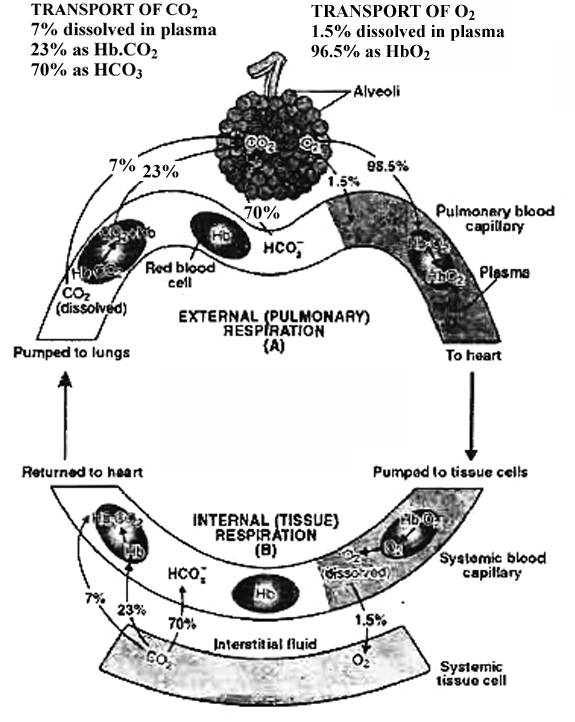
Release of CO2 in the alveoli of lung:
In the pulmonary capillaries, CO2 starts diffusing out into alveoli.
Carbamino-Hb spits into CO2 and Hb. As Hb of RBC takes up O2, it releases H+ in RBC.
The H+ start combining with the available HCO3– in RBC to form H2CO3 which splits into H2O + CO2 and CO2 starts diffusing out (Reverse of the reactions).
As a result HCO3– from plasma starts moving in along concentration gradient and for ionic balance; Cl– start moving out.
This way CO2 is released into lungs.
Hamburger's Phenomenon:
HCO3-ions diffuse out into plasma and Cl– ions enter into the RBCs at the level of tissues (intemal respiration). This is known as "chloride shift" or "Hamburger phenomenon". At the level of external respiration or alveoli, Cl– move out as HCO3– move in this is called reverse of chloride shift.
Haldane's Effect
It is related to the transport of CO2 in the blood. It is based on the simple fact that oxyhaemoglobin behaves as strong acid and releases an excess of H+ ions which bind with bicarbonate (HCO3–) ions to form H2CO3 which dissociates into H2O and CO2.
Secondly, due to the increased acidity, CO2 loses the power to combine with haemoglobin and form carbamino-haemoglobin.
Effect of oxyhaemoglobin formation or dissociation on CO2 transport is called Haldane's effect
Regulation of Respiration
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
Regulation of Respiration
Respiration may be defined as the process in which oxygen is taken inside the body from the environment for the oxidation of food to release energy and the carbon dioxide so produced during oxidation is expelled out of the body.
The process of oxidation of food is very complex.
It involves a series of complex biochemical reactions and the released energy is stored in the form of ATP molecules.
However, for simplicity sake, the multistep reaction can be briefly expressed as follows:
![]()
Types of Respiration
1. Direct and Indirect Respiration
(a) Direct Respiration:
There is direct exchange of gases between the carbon dioxide of the body cells and oxygen of water and there is no blood for the transport of gases.
Exchange of gases occurs on the principle of diffusion.
It is found in unicellular organisms like aerobic bacteria and protists (e.g. Amoeba) and metazoans like sponges, coelenterates (e.g. Hydra), flatworms, roundworms and insects.
(b) Indirect Respiration:
There is no direct contact between the body cells and the surrounding air or water the source of oxygen is called respiratory medium.
It is found in larger and complex forms of animals.
These organisms have some specialised organs; gills (most of crustaceans, molluscs, insect larvae, all fishes and amphibians); lungs (snails, amphibians, all reptiles, birds and mammals).
In this the transportation of oxygen and carbondioxide between the respiratory organs and the body cells is brought about by the blood of the Circulatory system.
2. All physical and chemical reactions in which atmospheric air oxidises food in the body cells resulting in production of energy and liberation of CO2 are included in respiration.
It is of following types:
(a) Anaerobic respiration:
It occurs when nutrients are oxidised without using O2 (also called fermentation).
In yeast, glucose forms ethyl alcohol and CO2, In bacteria and muscles, glucose is converted into lactic acid.
Endoparasites also respire anaerobically.
Anaerobic respiration is low energy yielding process.
In mature RBCs also anaerobic respiration occurs due to loss of mitochondria along with other cell organelles.
(b) Aerobic respiration:
Cells utilize O2 for oxidising nutrients.
O2 is used either from atmospheric air or from water.
It involves:
(i) External respiration: gaseous exchange between blood and air (or water) of O2 and CO2,
(ii) Transport of gases to the tissues.
(iii) Internal respiration : gas.eous exchange between blood and tissues.
(iv) Cellular respiration : oxidation of nutrients in the cells and liberation of energy.
Phases of Aerobic Respiration.
(i) External Respiration (Breathing or ventilation).
It is the exchange of oxygen of surrounding gaseous or liquid medium and carbon dioxide of blood through a liquid medium by diffusion across the body surface or the respiratory surface. It is purely a physical process which depends upon the principle of diffusion and no energy is produced.
(ii) Internal Respiration.
It is the exchange of oxygen of blood and carbon dioxide of the body cells through tissue fluid at the cellular level. Internal respiration involves the energy production and is a physico-chemical process.
(iii) Cellular Respiration:
It is utilisation of O2 by cells for energy production and resultant release of CO2,
Disorders of Respiratory System
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
Disorders of Respiratory System
Asthma is a difficulty in breathing causing wheezing due to inflammation of bronchi and bronchioles.
Emphysema is a chronic disorder in which alveolar walls are damaged due to which respiratory surface is decreased.
One of the major causes of this is cigarette smoking.
Occupational respiratory disorders:
In certain industries, especially those involving grinding or stone-breaking, so much dust is produced that the defense mechanism of the body cannot fully cope with the situation.
Long exposure can give rise to inflammation leading to fibrosis (proliferation of fibrous tissues) and thus causing serious lung damage.
Workers in such industries should wear protective masks.
 ACME SMART PUBLICATION
ACME SMART PUBLICATION
