Human Excretory System
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
HUMAN EXCRETORY SYSTEM
1. In humans, the excretory system consists of a pair of kidneys, one pair of ureters, a urinary bladder and a urethra.
Kidneys: Kidneys are reddish brown, bean shaped structures situated between the level of last thoracic and 3rd Lumbar vertebra close to the dorsal inner wall of the abdominal cavity. Each kidney measures about 10 -12 cm long, 5 -7 cm in width and 2 -3 cm thick. It weighs about 120 -170 g in adults. Left kidney is little higher than the right one because of more space being occupied by the liver on right side.
2. Towards the centre of the inner concave surface of the kidney is a notch called hilum through which ureter, blood vessel and nerve enters. Inner to the hilum is a broad funnel shaped space called the renal pelvis.
Kidney is covered by 3 protective layers which are as foillows :
1. Renal Capsule: It is innermost, tough protective cover made up of white fibrous connective tissue, with few elastic fibres and few muscles.
2. Adipose Capsule: It is the middle cover involving adipose tissue and acts as shock absorber.
3. Renal Fascia: It is the outermost fibrous cover linking it with the abdominal wall.
As the kidneys are fused with the body wall on the dorsal side, peritoneal cover is present only on the ventral side. This arrangement is called Retroperitoneal arrangement.
Internal Structure of Kidney
A longitudinal section of the kidney shows two functional layers, outer renal cortex and inner renal medulla.
(a) Renal Cortex: It is the outer part which is dark in colour and granular in nature.
(b) Renal Medulla : It is the inner part which is lighter in colour and striated in nature. Medulla has 8 -18 conical renal pyramids. They actually represent multilobular condition of foetal kidney.
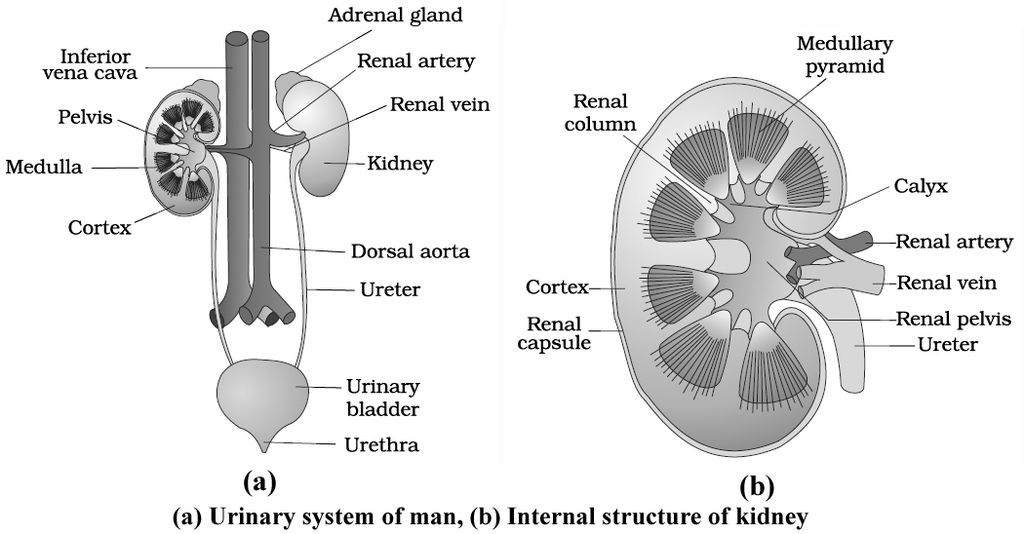
Each renal pyramid has a broad base towards the cortical side. Apex is pointed and is called renal papilla.
1-3 renal papillae project into a activity called minor calyx, which join up and form major calyces.
Cortex projects into medulla in the regions in between the pyramids and calyces, called renal columns of Bertini.
Interstitial fluid of medulla region has a higher osmotic concentration equal to some 1200 mosm/lt. due to higher quantity of two solutes, NaCl and urea.
Cortical region close to medulla is called juxtamedullary area.
The major calyces open into a broad funnel-shaped structure called renal pelvis placed inner to hilum.
It is lined by transitional epithelium.
It leads into ureter.
Structural and functional units of kidney are called nephrons or uriniferous tubules.
There are about 1 million nephrons in each kidney.
The number of uriniferous tubules decreases with age.
Ureters:
They are a pair of fine whitish distensible muscular tubes of 25 -30 cm length, about 3 mm in diameter.
Ureters develop from hilum part of the kidneys, descend along the abdominal wall, bend obliquely inwards and upwards to open in to urinary bladder in the region of trigone by oblique slits, one on each side.
Wall of ureter has 3 coats -extemal adventitia, middle muscular and inner mucosa, Muscular coat has three layers of smooth muscle fibres -outer longitudinal, middle circular and inner longitudinal.
Ureters are always undergoing peristalsis which helps in passing urine from kidney to urinary bladder.
Urinary Bladder:
It is a median pyriform sac which varies in shape, size and position according to the amount of urine contained in it.
The fully distended bladder becomes ovoid in outline.
Bladder has three parts -apex, fundus or body and neck. Body has a triangular area called trigone.
It has openings of ureters and an internal urethral orifice.
Neck region possesses two sphincters, involuntary internal sphincter and voluntary external sphincter.
Neck leads into urethra.
Wall of urinary bladder consists of three coats -outer adventitia, middle muscular and inner mucosa.
The muscle present in the middle muscular coat is also called detrusor muscle because it takes part in detrusion or pushing down of urine.
Muscular coat has involuntary circular muscles in the middle and involuntary longitudinal muscles on its either side.
Mucosa has loose connective tissue towards the side of muscular layer and transitional epithelium or urothelium towards lumen.
Adventitia is formed of soft connective tissue.
During the micturition, both the sphincters undergo relaxation.
Cerebral cortex direct the sphincter to relax and person undergoes urination.
Wall of urinary bladder is innervated by both sympathetic and parasympathetic nervous system.
Urethra:
It is present only in mammals. It starts from the neck of the urinary bladder and opens outside the body.
In female, it is short (2-4 cm), straight and concerned with the release of urine through an aperture called urethral orifice or urinary aperture present in the vulva in front of the vaginal aperture.
However, in male, it is quite long (20 cm), passes through the ejaculatory duct, prostate gland, cowper's glands and penis.
It is concerned with the release of urine as well as semen (sperms + glandular secretion) through an aperture called urinogenital aperture at the tip of the penis.
Blood Supply to Kidney
A renal artery enters each kidney and divides into many afferent arterioles which enter the Bowman's capsules and sub-divide to form glomerulus.
The glomerular capillaries rejoin to form efferent arteriole.
Efferent arteriole is narrower than afferent arteriole.
This raises blood pressure inside glomerulus.
Efferent arteriole further forms numerous peritubular capillaries in the cortex region around the proximal and distal convoluted tubules of the nephron.
It further forms vasa recta around the loop of Henle.
Blood from the vasa recta is released into the renal venule from where it escapes into renal vein.
Urine Formation
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
URINE FORMATION
Nephric excretion involves the formation of urine. Urine formation occurs in three steps -glomerular filtration, tubular reabsorption and tubular secretion.
1. Glomerular Filtration (Ultrafiltration):
Blood present in the glomerular 'capillaries is separated from the capsular space of Bowman's capsule by
(i) Endothelial covering of blood vessels.
(ii) Basement membrane of blood vessel.
(iii) Basement membrane of visceral layer
(iv) Visceral layer or inner wall of Bowman's capsule.
Therefore, the actual barrier between blood and capsular space consists of two basement membranes which are, however, permeable to small sized molecules.
Development of Filtration Pressure:
Blood flows through glomerular capillaries under a pressure.
The pressure is due to two reasons:
(i) Wider diameter of afferent arteriole as compared to diameter of efferent arteriole.
(ii) Natural arterial pressure caused by pumping activity of heart. Blood pressure in glomerular blood is about 60 mm Hg, this is called glomerular hydrostatic pressure (GHP). Osmotic concentration of proteinaceous content of glomerular blood is equivalent to 30 mm Hg, this is called blood colloidal osmotic pressure (BCOP). Pressure of interstitial fluid and pressure of renal filtrate is collectively called capsular hydrostatic pressure (CHP =20 mmHg). The pressure being exerted on glomerular blood for undergoing filtration is called glomerular filtration pressure (GFP). It is about 10 mm Hg.
or, GFP = GHP -(BCOP + CHP)
= 60 – (30 + 20) = 10 mmHg
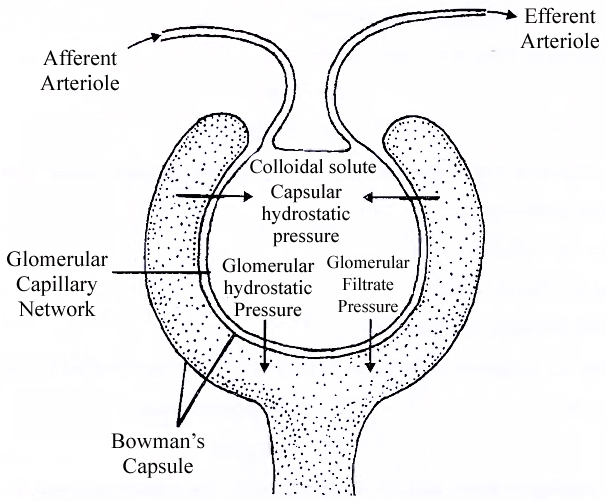
Ultrafiltration:
As there is net higher hydrostatic pressure of 10 mm Hg in the lumen of glomerular capillaries as compared to lumen of Bowman's Capsule, the filterable components of blood are passed out of the glomerular capillaries.
They pass through endothelial fenestrations, basement membranes and filtration slits of podocytes to enter the lumen of Bowman's capsule.
The phenomenon is called nephric or glomerular filtration.
About 1100-1200 ml of blood is put to filtration in the two kidneys every minute which constitutes roughly 1/5th of the blood pumped out by each ventricle of the heart in a minute.
It produces a glomerular or nephric filtrate of about 125 ml/min or 180 Uday.
The rate of filtration is called glomerular filtration rate or GFR.
Nephric filtrate consists of water, various electrolytes (Na+, K+, Ca2+, Mg2+, K+, PO43–), glucose, amino acids, hormones, vitamins, urea, creatinine, uric acid etc.
It is alkaline like blood but excludes large sized particles and structures like fats, proteins, platelets, leucocytes and erythrocytes.
Separation of small volume solutes from large volume solutes and components due to filtration through small sized pores or slits by the application of pressure is called ultrafiltration.
Autoregulation of Glomerular Filtration:
There are three methods by which renal blood flow and glomerular filtration rate (GFR) are automatically regulated.
(a) Myogenic Autoregulation:
A rise in blood pressure should normally increase blood flow through glomeruli.
However, stretching of the vascular wall increases passage of Ca2+ ions from extracellular fluid into the cells resulting in their contraction.
Contraction checks overstretching of vascular walls and raises vascular resistance so that rate of blood flow and GFR are brought down to normal.
(b) Juxtaglomerular Apparatus (JGA):
The apparatus becomes active when there is decrease in renal blood pressure or decrease in glomerular filtration rate (GFR).
It promotes release of renin from Juxta-glomerular cells.
Renin converts protein angiotensinogen into peptide angiotensin.
Angiotensin is a hormone that raises glomerular blood pressure through constricting efferent arterioles resulting in restoring GFR.
It also brings about release of aldosterone.
(c) Neural Control:
Blood vessels of the kidney are innervated by nerve fibres of the sympathetic nervous system.
When activated, the nerve fibres bring about constriction of renal arteries and cause decrease in renal blood flow as well as glomerular filtration rate.
Functions of the Tubules
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
Functions of the Tubules
Types of Nephron
A kidney has two types of nephrons-cortical and juxtamedullary. They are held together with the help of connective tissue
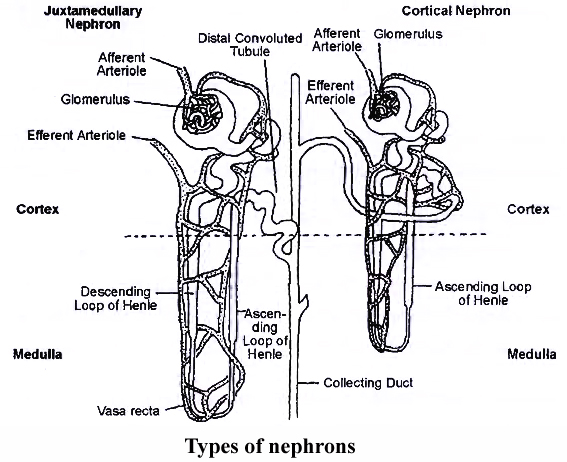
(a) Cortical Nephrons:
They constitute about 85%, of the total nephrons.
Cortical nephrons are smaller in size with major part lying in the cortex.
The tubule is much coiled.
Loop of Henle is short and extends into medulla to a short distance.
Vasa recta are absent or highly reduced.
Glomeruli lie in the outer cortex.
(b) Juxtamedullary Nephrons:
They are approximately 15% of the total and are present at the junction of cortex and medulla region of kidney.
They have large size, less coiling and a long loop of Henle.
Glomeruli occur in the inner cortex.
The long loops of Henle placed deep in the medulla.
Vasa recta occur over the loops of Henle.
Juxtamedullary nephrons become active during shortage of water.
They increase water reabsorption and, therefore, control the volume of plasma.
The system usually works under stress conditions.
Structure of Nephron (Renal Tubule, Uriniferous Tubule)
Nephron or uriniferous tubule is the structural and functional unit of kidney.
It is about 3 cm long and 20-60 mm in diameter. Each nephron consists of two parts -Glomerulus and renal tubule (Bowman's capsule, PCT, Henle's loop and DCT)
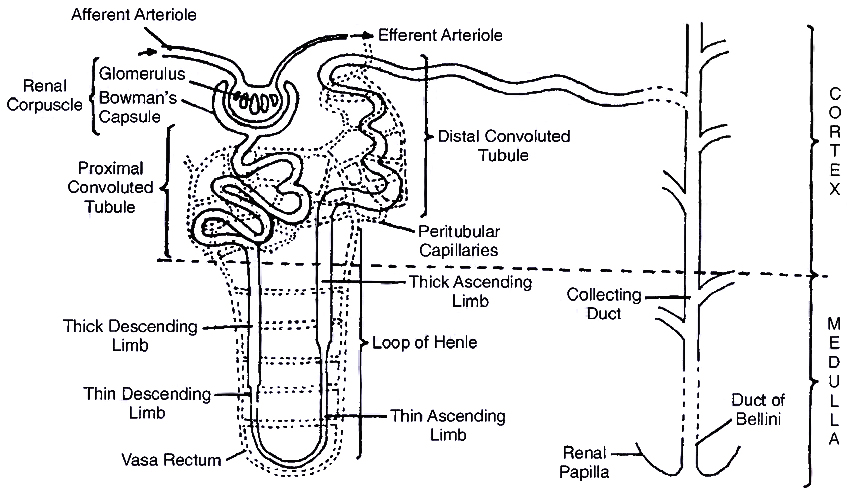
1. Bowman's Capsule:
It is blind double walled cup-shaped structure. The two walls of Bowman's capsule are inner visceral and outer parietal. Both are single layered and are supported over basement membrane.
(i) Visceral Layer (Inner Wall):
It consists of flat squamous epithelial cells on the periphery and specialised podocytes in the remaining part.
A podocyte has a number of interdigitated evaginations called pedicels or feet.
The pedicels rest over the basement membrane.
They enclose slit pores or filtration slits.
The diameter of these slits is about 25 nm.
Pedicels also possess contractile filaments which help in passage of filtrate through the filtration slits.
(ii) Parietal Layer (Outer Wall):
It consists of flat squamous epithelium.
The space between the two layers of Bowman's capsule is called lumen or capsular space.
Glomerulus:
It is a tuft of capillaries formed by fine blood vessels lying in the Bowman's capsule.
Glomerulus receives blood from an afferent arteriole.
Blood is taken away from the glomerulus by an efferent arteriole.
The latter has a narrower diameter than that of afferent arteriole.
Blood vessels of glomerulus are similar to those of blood capillaries in being covered by a single layer of endothelial cells.
However, they are 100-500 times more permeable with fenestrations or pores having a size of 50-100 nm.
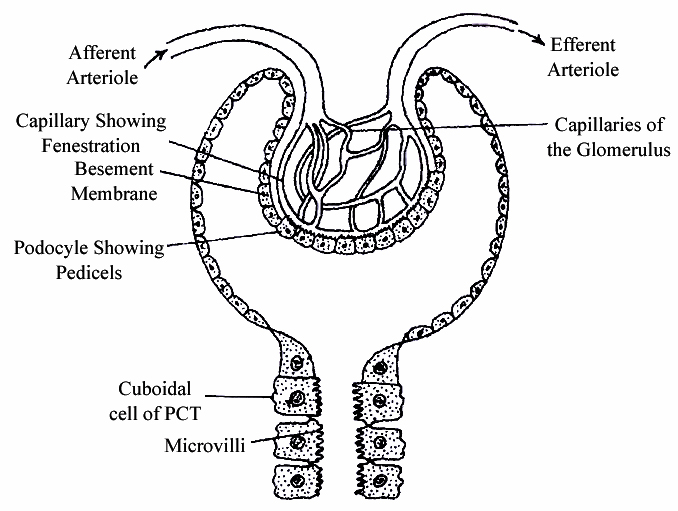
Malpighian body (renal corpuscle) : The complex formed by glomerulus, connective tissue and Bowman's capsule is called Malphighian body or renal corpuscle.
2. Proximal Convoluted Tubule (PCT):
Lower part of Bowman's capsule leads into proximal convoluted tubule.
The latter is present in the cortex.
It is twisted and surrounded by peritubular blood capillaries.
PCT is lined by cuboidal epithelium having brush borders with long microvilli for increasing absorptive area.
The cells contain abundant mitochondria and food reserve for providing energy to perform active absorption and secretion.
3. Loop of Henle:
Loop of Henle is made of two parallel limbs joined by curved base.
There is a descending limb and an ascending limb.
(i) Descending Limb:
Thick segment constitutes about four-fifth of the descending limb.
It lies both inside cortex and medulla.
The cells lining it are cuboidal.
They have sparse microvilli and fewer mitochondria indicating that active absorption and secretion are absent.
Thin segment is narrow part of descending limb.
It lies in the medulla and is lined by flat epithelial cells having sparse microvilli and few mitochondria.
Thin segment gets curved to become part of ascending limb.
(ii) Ascending Limb:
Ascending limb consists of thin segment in the proximal part and thick segment afterwards.
Thin segment is lined by flat epithelial cells which allow passive diffusion of some solutes (e.g., Na+, Cl–) depending upon their concentration gradient.
Thick segment of ascending limb is wider and lined by cuboidal cells having microvilli as well as mitochondria.
Thick ascending segment is involved in active secretion of NaCl in the medulla.
Vasa Recta : Loop of Henle is covered by a stair case of network of blood capillaries arising from efferent glomerular arteriole called vasa recta. It forms a counter-current system with the loop of Henle having ascending branch in the area of descending limb and descending branch in the area of ascending limb.
4. Distal Convoluted Tubule (OCT):
Distal convoluted tubule is highly coiled part of nephron and lies close to Malpighian body.
The epithelial lining of the distal convoluted tubule consists of cuboidal cells having sparse microvilli and deep mitochondria.
Distal convoluted tubule is covered by peritubular blood capillaries.
The last part of distal nephron is nearly straight, called connecting or junctional tubule and open into collecting duct.
Collecting Ducts:
Each nephron opens into a wider collecting tubule in the area of cortex.
Collecting tubules are lined by specialized cuboidal epithelium with very few microvilli.
They open into still wider collecting ducts.
Collecting ducts enter medulla and form ducts of Bellini.
The ducts run through renal pyramids.
Mechanism of Concentration of the Filter
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
Mechanism of Concentration of the Filter
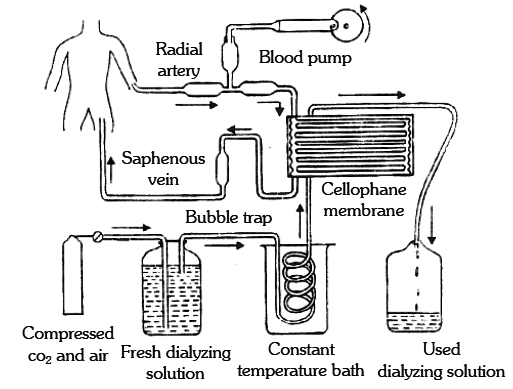
KIDNEY TRANSPLANTATION
When both the kidneys are completely damaged kidney transplantation is done.
The world's first successful organ transplant was kidney transplantation which was undertaken by David Hume and Joseph Kelly at the Peter Bent Brigham Hospital in Boston in 1954.
The recipient was Richard Heerick who lived for a further eight years. The first kidney transplant in India was performed on Dec. 1, 1971 at the Christian Medical College, Vellore (Tamil Nadu) on a 35 year old patient named Shanmughan.
Most patients need to be dialysed before transplantation to avoid fluid overload and hyperkalaemia after the operation.
Antibiotics and immunosuppressive drugs are given before the operation.
Postoperative care is very essential.
Regulation of Kidney Function
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
REGULATION OF KIDNEY FUNCTION
Control by Antidiuretic Hormone (ADH):
ADH, produced in the hypothalamus of the brain and released into the blood stream from the pituitary gland, enhances fluid retention by making the kidneys reabsorb more water.
The release of ADH is triggered when osmoreceptors in the hypothalamus detect an increase in the osmolarity of the blood above a set point of 300 mosm L–1.
In this situation, the osmoreceptor cells also promote thirst.
Drinking reduces the osmolarity of the blood, which inhibits the secretion of ADH, thereby completing the feedback circuit.
Control by Juxtaglomerular Apparatus (JGA):
Juxtamedullary nephrons help in retaining Na+ ions in high concentration in the interstitial fluid between the nephrons.
JGA operates a multi hormonal Renin-Angiotensin Aldosterone System (RAAS).
The JGA responds to a decrease in blood pressure or blood volume in the afferent arteriole of the glomerulus and releases an enzyme, renin, into the blood stream in the blood, renin initiates chemical reactions that convert a plasma protein, called angiotensinogen, to a peptide, called angiotensin II, which works as a hormone.
Angiotensin II is powerful constrictor of arterioles; one of the most potent vasopressor substances known.
Angiotensin II increases blood pressure by causing efferent arterioles to constrict.
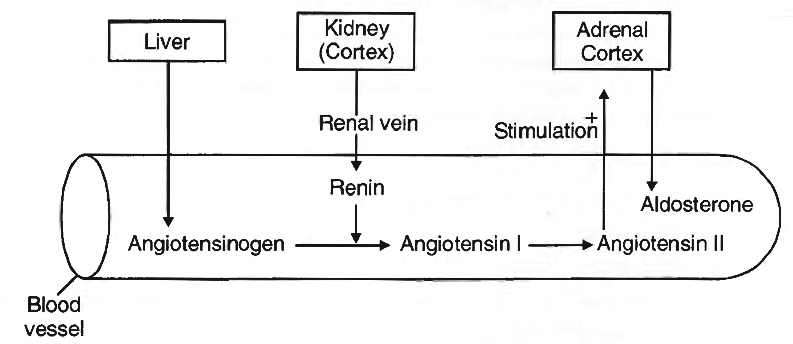
It also increases blood volume in two ways : firstly, by signalling the proximal convoluted tubules to reabsorb more NaCl and water, and secondly, by stimulating the adrenal gland to release aldosterone, a hormone that induces the distal convoluted tubule to reabsorb more Na+ and water.
This leads to an increase in blood volume and pressure, completing the feedback circuit by supporting the release of renin.
Atrial Natriuretic Factor (ANF), opposes the regulation by RAAS. (Renin -Angiotensin -Aldosterone System).
The wall of the atria of the heart release ANF in response to an increase in blood volume and pressure.
ANF inhibits the release of renin from JGA. This inhibits the reabsorption of Na+ by the collecting duct and reduces release of aldosterone from adrenal gland.
It also increases excretion of Na+ in urine.
Micturition
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
Micturition
Voiding or expulsion of urine stored in the urinary bladder is called micturition.
Urinary bladder gets gradually filled up with the urine.
Though the capacity of urinary bladder is above 800 ml, but as the volume is around 500 ml, its wall gets stretched.
Urine formed by nephrons is ultimately carried to the urinary bladder where it is stored till a voluntary signal which is initiated by the stretching of urinary bladder as it gets fill with urine.
Stretch receptors generate nerve impulse that is carried by sensory neuron to brain producing the sensation of fullness.
This initiates the autonomic reflex (parasympathetic involving sacral spinal nerves) resulting in contraction of detrusor muscles of urinary bladder and inhibition of motor impulse of voluntary, striated external sphincter, making it relaxed; and urine comes out.
Micturition can be initiated voluntarily also by contracting the abdominal muscle which applies pressure over urinary bladder, activating the stretch receptors.
Role of other organs in Excretion
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
ORGANS IN EXCRETION
Lungs:
The lungs help in removing CO2 and water. Lungs eliminate around 18 L of CO2 per hour and about 400 ml of water per day in normal resting condition.
Water loss will increase in cold dry climatic condition and will decrease in hot, humid climate. Different volatile material are also readily eliminated through lungs.
Skin:
Skin contains large number of sweat glands richly supplied with blood capillaries, from which they excrete sweat and some metabolic wastes.
Since the skin sends out plenty of water and small amount of salts, hence it serves as an excretory organ.
Sebaceous glands in skin eliminate sebum which contains waxes, sterols, some hydrocarbons & fatty acids.
Liver:
It produces bile pigments which are metabolic wastes of haemoglobin of dead R.B.C's.
Liver is also the main site for elimination of cholesterol, inactivated products of steroid hormones, some vitamins and many drugs.
Large Intestine:
Epithelial cells of large intestine excrete Ca2+, Mg2+, Fe2+ into the lumen of intestine and comes out along with faecal matter.
Disorders of the Excretory System
- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
Disorders of the Excretory System
1. Nephritis: The infection is caused by bacteria which results in inflammation of the kidney.
2. Glomerulonephritis: Inflammation of glomeruli.
3. Pyelonephritis: Inflammation of the tissue of kidneys in the pelvis region.
4. Cystitis: Inflammation of the urinary bladder.
5. Renal Calculi: Stone or insoluble mass of crystallized salts (oxalate etc.) formed within kidney.
6. Polyurea: Amount of urine passed out is more.
7. Uremia: The concentration of urea is increased in blood.
8. Alkaptonuria: It is a genetic disease in which homogentisic acid in excreted out with urine.
9. Pyuria: Presence of pus in the urine.
10. Glycosuria: Presence of glucose in urine.
11. Haematuria: Presence of blood in the urine.
12. Inulin is a fructan storage polysaccharide. It is not metabolised in human body and is a readily filtered through kidneys. It is therefore used in testing kidney function, especially glomerular filtration rate.
13. Tubular maxima: The maximum amount of substance that can be retained in blood and beyond which it will be excreted in urine.
 ACME SMART PUBLICATION
ACME SMART PUBLICATION
