- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
BLOOD
Blood is a fluid connective tissue.
Its cells are quite distinct from other connective tissue cells both in structure and functions.
The extracellular material in blood is a fluid devoid of fibres.
Fluids outside the cells are generally called Extracellular Fluids (ECF).
Blood is heavier than water.
The extracellular material in blood is a straw-coloured, slightly alkaline (pH =7.4) aqueous fluid called plasma.
Constituents, having characteristic forms, float in the plasma.
They are collectively called the Formed Elements of blood.
They include the blood cells and blood platelets.
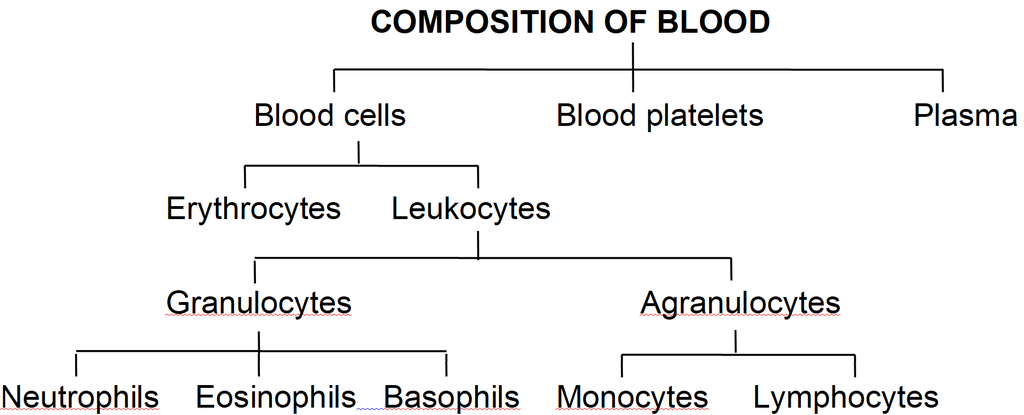
Blood cells are of two types-Erythrocytes and Leukocytes.
Blood circulates within blood vessels in higher animals.
But other extracellular fluids such as cerebrospinal fluid, interstitial fluid, lymph and aqueous humour occur outside blood vessels.
PLASMA
Plasma contains three major classes of plasma proteins viz. serum albumin, serum globulins and fibrinogen.
Plasma proteins serve as a source of proteins for tissue cells.
Tissue cells may utilise plasma proteins for forming their cellular proteins.
Additionally, albumin and globulins retain water in blood plasma by their osmotic effects.
A fall in plasma proteins leads to movement of excessive volumes of water from blood to tissues.
That is why hands and feet get swollen with accumulated fluid (oedema) in persons suffering from dietary deficiency of proteins.
Albumins and globulins also transport many substances such as thyroxine and Fe3+ in combination with them.
One class of globulins, called immunoglobulins, act as Antibodies.
Plasma proteins also maintain the blood pH by neutralising strong acids and bases.
Thus, they act as Acid-Base-Buffers.
It is slightly alkaline non-living inter-cellular substance which constitutes about 60% part of the blood.
It is a pale yellow but transparent and clear fluid.
Composition of Plasma. Plasma forms 55-60% by volume of blood.
1.Water-Water alone forms about 90% to 92% of the plasma. Solids form about 8% of the plasma.
2.Mineral Salts -These are chlorides, bicarbonates, sulphates and phosphates of sodium, potassium, calcium, iron and magnesium. All salts constitute about 0.9% of plasma. Buffer of the blood is sodium bicarbonate.
3.Nutrients - These include glucose, fatty acids, phospholipids, cho'lesterol, fats, aminoacids, nucleosides, etc. Mineral salts have been mentioned above.
4.Plasma proteins -They constitute about 7 to 8% of plasma. These mainly include albumin 4.4% , globulin 1.5 to 2%, prothrombin and fibrinogen both 0.3%.
5.Defence proteins - Immunoglobulins which act as antibodies and some other substances, such as lysozyme and properdin (a large protein) are always found in the plasma. They destroy bacteria, viruses and toxic substances that may enter into the blood from outside.
6.Excretory substances - These include ammonia, urea, uric acid, creatinine, etc.
7.Dissolved gases - Water of blood plasma contains oxygen, carbon dioxide and nitrogen in dissolved form.
8.Anticoagulant - Blood plasma contains a conjugated polysaccharide, heparin which prevents coagulation of blood inside blood vessels.
9.Hormones - These are secreted and released in blood by endocrine glands.
10.Vitamins and Enzymes-Different kinds of vitamins and enzymes are present in the blood plasma.
Functions of Blood plasma-
These can be summarised as under (i) transport, (ii) retention of fluid in blood, (iii) maintenance of blood pH, (iv) body immunity, (v) prevention of blood loss, (vi) conducting heat to skin for dissipation and (vii) uniform distribution of heat all over the body.
Blood Glucose
Glucose is mainly absorbed in the small intestine.
Glucose is also absorbed in the stomach.
After absorption glucose reaches the blood.
Excess of glucose is converted into glycogen by insulin hormone in the liver and muscles.
Whenever it is required, glycogen is changed back into glucose by glucagon hormone.
Usually blood glucose level is about 80-100 mg per 100 ml of blood, 12 hours after a normal meal.
But its concentration rises soon after a carbohydrate rich diet.
If blood glucose level exceeds 180 mg per 100 ml, it starts appearing in urine.
This condition is called glucosuria.
Fasting glucose is 70 -110 mg/dl. Glucose PP1 is 110 -140 mg/dl.
If it is higher, it causes diabetes mellitus (hyperglycemia).
If it is less, it causes hypoglycemia (less amount of glucose in blood).
Blood Cholesterol
Usually cholesterol is considered a harmful substance. But it is quite useful in limited amount.
Cholesterol is used in the synthesis of biomembranes, vitamin D, bile salts and steroid hormones.
Its normal amount is 80 -180 mg in 100 ml of blood plasma.
Cholesterol comes in the blood plasma either by intestinal absorption of fats or by the synthesis from the liver or by both.
Saturated fats such as ghee and butter increase cholesterol level in the blood.
Increased blood cholesterol may lead to its deposition in the internal wall of the blood vessels like arteries and veins which causes high blood pressure and heart problems.
Functions of Plasma Proteins
1. Prevention of blood loss - Fibrinogen and prothrombin playa role in blood clotting.
2. Retention of fluid in the blood - Albumin helps in osmotic balance.
3. Body immunity - Certain globulins called immunoglobulins (glycoproteins) act as antibodies in blood and tissue fluid. Antibodies belong to a class of proteins called as immunoglobulins.
4. Maintenance of pH - Plasma proteins serve as acid-base buffers. It means they maintain pH of the blood by neutralizing acids and bases.
5. Transport of certain materials - Thyroxine (hormone) is bound to albumin or specific globulin for transport in the plasma.
6. Distribution of heat - Plasma proteins help in uniform distribution of heat all over the body.
7. Enzymes - Some proteins acting as enzymes also occur in the plasma.
BLOOD CELLS
(i) Erythrocytes:
Erythrocytes (red blood corpuscles or RBC) are the most numerous of the formed elements of blood.
Their most important characteristic feature is the presence of hemoglobin, the red oxygen carrying pigment.
The total number of erythrocytes per microlitre (1 µl = 1mm3 =10–6) of blood is known as the Total Count of RBC.
It averages 5 millions and 4.5 millions in adult man and adult woman respectively.
The total count would be low in anaemia and after profuse bleeding.
On the contrary, the abnormal rise in the total count of RBC is called Polycythemia.
Anaemia is caused due to the deficiency of folic acid, vitamin B12 and haemoglobin.
The size and shape of erythrocytes vary in different classes of animals.
In fishes, amphibians, reptiles and birds, erythrocytes are usually nucleated, oval and biconvex. But in mammals they are non nucleated, biconcave and circular.
Only camel and llama possess oval red blood corpuscles.
Human erythrocytes measure 7-8 µm (1µm =10–6 m) in diameter and 2 µm thickness near the rim.
Old and damaged erythrocytes are phagocytosed and destroyed by macrophages.
The pigment part (porphyrin) of hemoglobin is then catabolised to the yellow pigment Bilirubin which is excreted in the bile.
The pale yellow colour of plasma is largely due to bilirubin.
If a sample of blood is rendered non-coagulable by adding potassium or sodium oxalate and then centrifuged at a high speed in a graduated centrifuge tube (hematocrit tube), the centrifugal force rapidly sediments the erythrocytes tothe bottom of the tube.
They become packed into a solid, red, bottom layer while plasma forms a clear, fiuid upper layer.
On the upper surface of the erythrocyte layer, leukocytes form a thin, buff-coloured layer.
From the graduations on the tube, the relative volume of erythrocytes may be read as a percentage of the total blood volume. This is called the Hematocrit Value or Packed Cell Volume.
It normally forms 45 percent of the blood volume.
RBC of mammals are circular, biconcave, non-nucleated except family camelidae. e.g. camel, which has non-nucleated and oval RBC. Largest RBCs are found in amphibia.
Smallest RBCs are found in mammals.
In mammals smallest RBCs are found in 'Musk Deer', Tragulus javanicus (1.5 µm).
In mammals, largest RBCs are found in elephant. (9.4 µJ).
Graveyard of RBC is spleen.
Life Span
Life span of RBC in man =120 days
Life span of RBC in frog = 100 days
Life span of RBC of rabbit = 80 days
Radioactive chromium method (Cr51) is used for estimation of life span of RBC.
Count of RBC
In embryo = 8.5 million/mm3
In Man = 5 to 5.5 million/mm3
In Woman = 4.5 million/mm3
Daily destruction of RBC = 1%
ESR (Erythrocyte sedimentation rate) : It is measured by Wintrobe's method. It is rate of settling down of RBC.
It is also estimated by Westergen's method.
ESR is very useful in diagnosing various diseases including tuberculosis, ESR in men is 0-5 mm/hour and in women it is 0-7 mm/hr in Westergen method.
Haemocytometer: It is instrument for counting the number of both WBCs and RBCs.
Rouleaux: In resting and slow flowing blood, the RBCs aggregate to form rouleaux (the RBCs are piled on top of each other). Fibrinogen favours rouleaux formation.
Bone marrow: It is the main site for formation of RBC. Volume of bone marrow at the time of birth is 70 ml. In adult volume of bone marrow is 4,000 ml.
Structure of RBC of man: Biconcave non-nucleated bounded by Donnan's membrane (plasma membrane of RBC). Haemoglobin is filled in RBC which is respiratory pigment.
Normal Range of Hb
Infants 16.5 ± 3.0 g/dl (dl = deciliter)
Children 3 months 11.0 ± 1.5 g/dl
Children 3 to 6 years 12.0 ± 1.0 g/dl
Children 10 to 12 years 13.0 ± 1.5 g/dl
Men 15.5 ± 2.5 g/dl
Women 14.0 ± 2.5 g/dl
Structure of Haemoglobin:
Each molecule of haemoglobin contains 4 molecules of haem and 1 molecule of globin.
These are attached by co-ordinate bonds.
Haem is protoporphyrin compound and has 4 pyrrole groups jointed together to form ring structure.
In Hb, Fe is present in (Fe++) Ferrous form.
Haem is 5% & Globin is 95%. Globin is made of 4 polypeptide chains.
(ii) Leukocytes:
Leukocytes (white blood corpuscles or WBC) are devoid of hemoglobin and are consequently colourless.
Leukocytes are nucleated blood cells.
They are of two major classes : granulocytes (with cytoplasmic granules) and agranulocytes (without granules).
Granulocytes are of three types, viz. neutrophils, eosinophils and basophils, each with lobed nucleus.
Agranulocytesare of two types, viz. lymphocytes and monocytes.
Neutrophils and monocytes protect the body against microbes by phagocytosing them.
Lymphocytes secrete antibodies in the blood to destroy microbes and their toxins.
The number of leukocytes per microlitre (1 µl = 1 mm3 = 10–6) of blood is called the Total Count of WBC.
It is 6000-8000/mm3 of blood normally.
It may rise abnormally in acute infections (e.g., pneumonia), inflammations (e.g. appendicitis) and malignancies (e.g., leukemia).
In some conditions such as folic acid deficiency, the total count falls abnormally (leukopenia).
The total count of WBC is also of diagnostic value in many diseases.
Monocytes have kidney shaped nucleus.
The process by which monocytes and neutrophils squeeze out through thin capillary walls is Diapedesis.
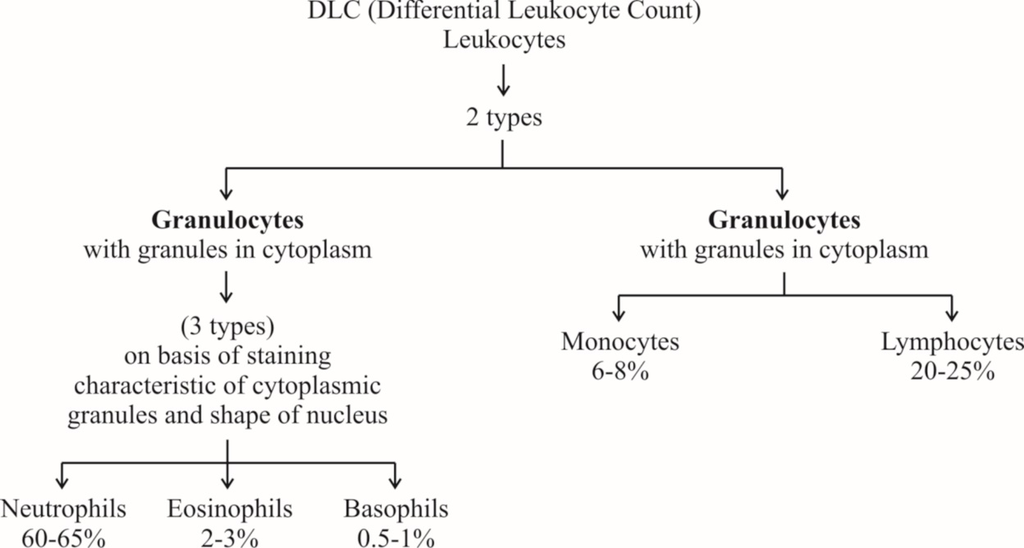
(a) Neutrophils: They are maximum in number, stain equally with both basic and acidic dyes and have many lobed nucleus, granules are in abundance in cytoplasm and help in phagocytosis.
(b) Eosinophils: They have bilobed nucleus, stain with acidic stains. Their number increases during allergic reactions (Eosinophilia).
(c) Basophils: They stain with basic dyes. Their nucleus is 'S' shaped. Coarse granules are few in the cytoplasm. Basophils release heparin and histamine in the blood and have a function similar to the mast cells.
(d) Lymphocytes have large and rounded nucleus. The cytoplasm forms a thin peripheral film. They have their stem cells in the bone marrow and are differentiated in the bone marrow or in the thymus. Lymphocytes are of two types, B-lymphocytes and T-lymphocytes.
B-lymphocytes produce antibodies against antigens and they mature in the bone marrow.
(e) Monocytes are the largest leucocytes (12-15 µm). The nucleus is kidney shaped. They are produced from bone marrow monoblast cells. They help in phagocytosis.
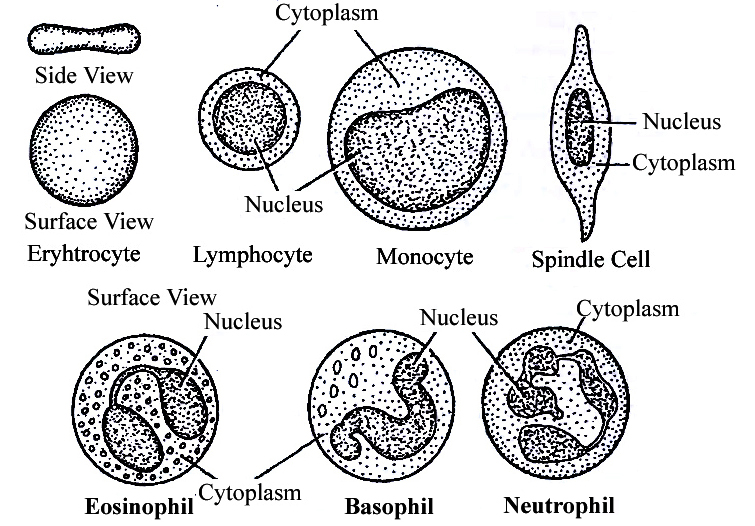
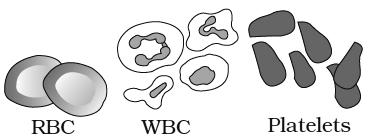
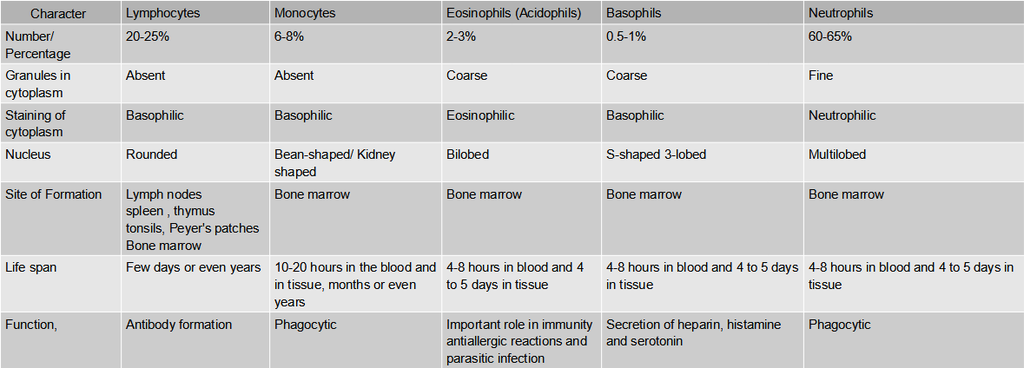
Table: Differences between different types of Leucocytes
(iii) Blood platelets:
Also called thrombocytes, blood platelets are non-nucleated, round or oval, biconvex disc-like bodies.
They are 2-3 micrometres in diameter and their number normally varies from 0.15 to 0.35 million/mm3 or 150000 -350000 platelets/mm3.
They bud off from the cytoplasm of very large Megakaryocytes of the bone marrow.
Their normal life-span is about a week.
When a blood vessel is injured, platelets get clumped at the injured spot and release certain chemicals called Platelet Factors.
These promote blood coagulation.
Thrombocytopenia is decrease in platelet count and Purpura is a group of bleeding diseases due to thrombocytopenia.
BLOOD COAGULATION
When blood oozes out of a cut, it sets into gel within a few minutes. This is called coagulation.
Coagulation is brought about by hydrolysis of soluble fibrinogen of plasma to insoluble fibrin.
This is catalysed by an enzyme called thrombin.
Fibrin precipitates as a network of fibres.
This network traps many blood cells, particularly RBCs, to form a red solid mass called the Blood Clot.
The clot seals the wound in the vessel to stop the bleeding.
The straw coloured fluid left after clotting of blood, is called Serum.
The serum cannot be coagulated as it lacks fibrinogen.
Thrombin occurs in normal blood as an inactive globulin called Prothrombin.
It must be activated to thrombin before blood coagulation can occur.
In case of injury to a blood vessel, coagulation promoting substances called Thromboplastins are released into the blood from clumped platelets and damaged tissues.
Thromboplastins help in the formation of the enzyme Prothrombinase.
This enzyme hydrolyses prothrombin to thrombin to initiate coagulation.
Ca2+ ions are essential for both activation and action of thrombin.
Blood normally contains an anticoagulant, Heparin which prevents activation of prothrombin, Heparin is released from mast-cell granules.
Blood also contains Antithrombin which inhibits any thrombin formed accidentally.
Blood drawn from a blood vessel can be kept uncoagulated by adding a pinch of oxalate (sodium or potassium oxalate) to it.
Oxalate precipitates Ca2+ and consequently prevents coagulation.
Chilling of blood also delays coagulation because lesser temperature depresses the action of coagulation promoting enzymes.
ABO Blood cloting factor:
Karl Landsteiner reported for the first time ABO blood groups in human beings.
A. B and O blood groups were discovered by Landsteiner (1900) while AS blood group was found out by de Castello and Steini (1902).
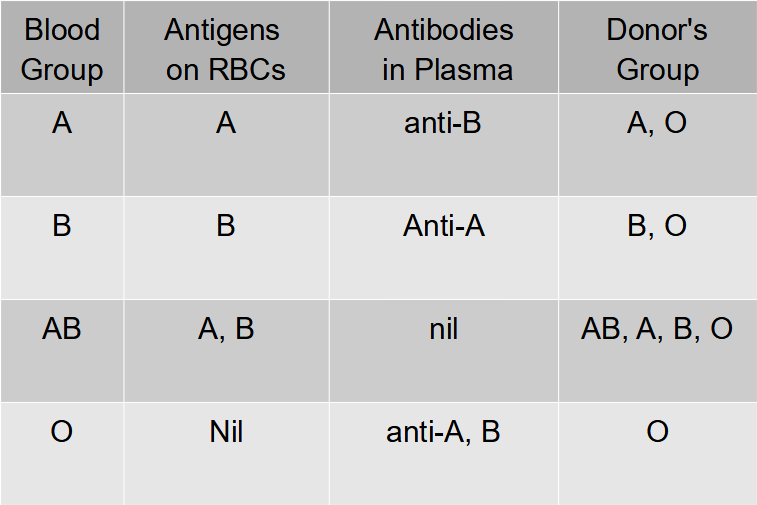
Agglutinogens (antigens) are present on the surface of red blood corpuscles and agglutinins (antibodies) are found in the blood plasma. Both antigens and antibodies are proteins.
When two different type of blood are mixed, the red blood corpuscles form a clump.
The clumping of red blood corpuscles is called agglutination.
Clotting Factors:
13 factors help in blood clotting.
These factors are mainly produced in liver.
Vitamin K is required in the synthesis of these clotting factors.
These factors are represented in Roman number.
I – Fibrinogen
II – Prothrombin
III – Thromboplastin
IV – Ca+2 (cofactor in each step of blood clotting)
V – Proaccelerin
VI – Accelerin (Rejected)
VII – Proconvertein
VIII – AHG Anti Haemophelic Globin (Absent in Haemophilia-A)
IX – Christmas factor
X – Stuart factor
XI – PTA (Plasma Thormboplastin Anticedent)
XII – Hagman factor
XIII – FSF Factors (Fibrin stabilizing factor) (Laki Lor and factor).
Other natural anticoagulants are
Hirudin – found in leech.
Anophelin – found in female Anophelese.
Lampredin – found in Peteromyzon (Lamprey)
Cumerin – obtain from plants
Warfarin – obtain from plants
To collect blood in bottle in blood bank artificial anticoagulants are used like
Sodium citrate
Sodium oxalate
EDTA (Ethylene diamine tetra acetic acid)
These chemicals act as Calcium binding units and remove Ca+2 ions from blood.
Blood group
Agglutination is due to the interaction of antigens and antibodies.
There are two kinds of antigens that are named A and B.
There are also two kinds of antibodies which are called a and b.
The antigen A and antibody a are incompatible (antagonistic) and cause self clumping and cannot exist together.
Similarly, the antigen B and antibody b are incompatible and cause self clumping and cannot exist together.
Thus, A and b can exist together and B and a can exist together.
The corpuscle factors A and B can occur together if their antagonistic plasma factors a and b are not present.
The plasma factors a and b can occur together if their antagonistic corpuscle factors A and B are absent.
Rh Factor
Another-antigen, the Rh antigen similar to one present in Rhesus monkeys (hence Rh), is also observed on the surface of RBCs of majority (nearly 80 per cent) of humans.
In India % ratio of Rh is
Rh+ – 97%
Rh– – 3%
In World
Rh+ – 80%
Rh– – 20%
Such individuals are called Rh Positive (Rh+ve) and those in whom this antigen is absent are called Rh negative (Rh-ve).
An Rh-ve person, if exposed to Rh+ve blood, will form specific antibodies against the Rh antigens.
Therefore, Rh group should also be matched before transfusions.
A special case of Rh incompatibility (mismatching) has been observed between the Rh-ve blood of a pregnant mother with Rh+ve blood of the foetus.
Rh antigens of the foetus do not get exposed to the Rh-ve blood of the mother in the first pregnancy as the two bloods are well separated by the placenta.
However, during the delivery of the first child, there is a possibility of exposure of the maternal blood to small amounts of the Rh+ve blood from the foetus.
In such cases, the mother starts preparing antibodies against Rh antigen in her blood. In case of her subsequent pregnancies, the Rh antibodies from the mother (Rh-ve) can leak into the blood of the foetus (Rh + ve) and destroy the foetal RBCs.
This could be fatal to the foetus or could cause severe anaemia and jaundice to the baby.
This condition is called erythroblastosis foetalis.
This can be avoided by administering anti-Rh antibodies to the mother immediately after the delivery of the first child.
 ACME SMART PUBLICATION
ACME SMART PUBLICATION
