- Books Name
- ACME SMART COACHING Biology Book
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 11
- Subject
- Biology
CONNECTIVE TISSUE
All connective Tissue in the body are developed from Mesoderm.
O. Hartwig called them Mesenchyme because they originated from embryonic mesoderm.
Only connective Tissue constitute 30% of total body weight.
(Muscle – 50%, Epithelium – 10% Nervous – 10%)
On the basis of matrix connective tissue is of 3 types -
1. Connective Tissue Proper – Matrix soft and fibrous
2. Connective Tissue Skeleton – Dense and mineralized matrix. Due to deposition of minerals it becomes hard.
3. Connective tissue Vascular – Liquid and fibres free matrix
Concept Builder
1. Connective Tissue Proper
Connective Tissue Proper is composed of three components (A) Different types of cells, (B) Fibres, (C) Matrix.
(A) Cells of connective tissue proper
Fibroblast cells :
Largest cell of connective tissue proper.
Maximum in number.
Cell body and nucleus both are oval shaped.
Branched cytoplasmic process arise from these cells so they appear irregular in shape.
Rich in rough ER because main or primary function is to produces fibres. Fibres are composed of protein.
Chief matrix producing cells.
Old fibroblast cells (fibrocyte) are inactive cells.
These are also considered as undifferentiated cells of conn. Tissue because they can be modified into Osteoblast & Chondrioblast cells to produce bone & cartilage.
Function : (1) To produce fibres (2) To secrete matrix.
Plasma Cell - Cart Wheel Cell
Less in number
Amoeboid in shape
Chromatin material is arranged like spokes in wheel so they are also called as Cart wheel cells.
According to research these cells are formed by the division of lymphocytes. So they are also called as clone of lymphocytes.
Function : Produce, Secrete & transport antibody.
Mast cells/Mastocytes
Numerous , amoeboid and small in size.
Structurally and functionally similar to basophils.
2-3 lobed S-shaped nucleus
Cytoplasm contains basophilic granules which can be stained with basic dye Methylene Blue.
It is important cell of connective tissue proper as they perform important functions.
(a) Histamine – Histamine is a protein, a vasodilator
Increase permeability of blood capillaries.
Take part in allergy and inflammatory reactions.
(b) Serotonin -
Also called as 5-Hydroxy tryptamine
It is a protein, a vasoconstrictor & decrease blood circulation but increases blood pressure.
At the site of cut or injury serotonin decrease blood loss.
(c) Heparin –
A mucopolysaccharide, a natural anti-coagulant, prevents clotting of blood in blood vessels by preventing the conversion of prothrombin into thrombin.
Adipose Cells/Fat Cells
Oval shaped stores fat.
Fat is collected in the form of fat globule formed by the fusion of small oil droplets.
On the basis of number of fat globules adipocytes are of two types.
(a) Monolocular adipocytes/ White fat tissue-cell
In these cells single large and central fat globule is present.
nucleus & Cytoplasm is peripheral and Cytoplasm is less in amount.
Due to compression of fat globule, nucleus become flattened in shape . These adipocytes form White Fat.
(b) Multilocular adipocytes/Brown fat tissue cell
In these cell 2-3 fat globules are distributed in the cytoplasm around nucleus
Cytoplasm is more in quantity.
Nucleus is rounded & found in the centre
These adipocytes form Brown Fat.
Mesenchymal Cells
Less in numbers. Small sized with cytoplasmic process having irregular shape.
Oval shaped nucleus
These are undifferentiated cells of connective tissue because they can transform into any cell of connective Tissue proper. (Totipotent in nature)
Function : To form other cells of connective tissue.
Macrophages/Histeocyte/Clasmatocytes.
– It is 2nd largest in size and in number.
– Amoeboid in shape with bean or kidney shaped nucleus.
– Cytoplasm quantity is more agranular but due to presence of a greater number of lysosomes it appears granular.
– Phagocytic in nature, destroy bacteria & viruses by phagocytosis. They arise by the fusion of monocytes
– Also called as scavenger cells of connective tissue because they destroy dead or damaged cells to clean connective tissue.
- Macrophages are named differently in different organs.
Lung – Dust cells
Liver – Kupffer cells
Blood – Monocytes
Brain – Microglial cells
Thymus gland – Hessels granules
Spleen – Reticular cells
Lymphocytes
Less in number and small in size having amoeboid shape.
A large nucleus is present cytoplasm is present as peripheral layer. Cytoplasm quantity is less.
Produce, transport & secretes antibodies.
They divide to form plasma cells of connective tissue proper.
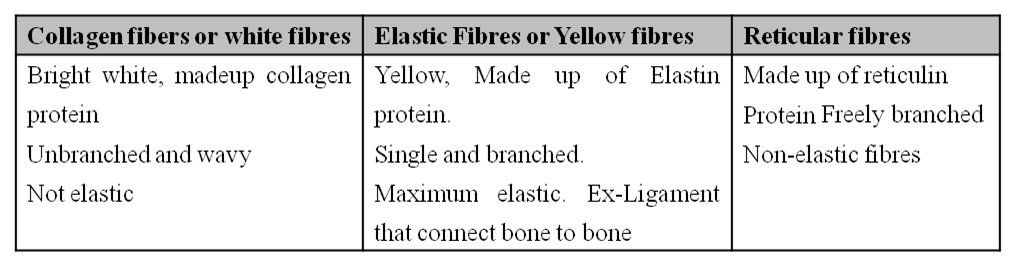
(B) FIBRES
Collagen fibres (White fibres)
They are shining white fibres composed of collagen protein (Tropocollagen).
It is present in maximum quantity in vertebrates, (only collagen fibres constituted one third part of connective tissue fibres in human beings.)
They are wavy & tough fibres always arranged in bundle called fascia.
On boiling they convert into gelatin.
They can be digested by Pepsin enzyme.
Elastic fibres – (Yellow fibres)
Precursor in colour and composed of elastin protein.
They are branched fibres but always arranged singly. Branches of these form network.
In these fibres maximum elasticity is present.
They are highly resistant to chemicals.
When boiled they do not dissolve.
They can be digested by trypsin enzyme.
Reticular Fibres: -
Precursor of Collagen fibres, delicate with no elasticity
Also known as Arzyrophil fibre since they can be stained with silver salts.
They are composed of recticulin protein highly branched fibres which always form dense network.
These are mainly distributed in lymphoid organs like spleen or lymph nodes.
 (C) MATRIX
(C) MATRIX
Matrix is composed of Mucopolysaccharide which is present in the form of Hyaluronic acid.
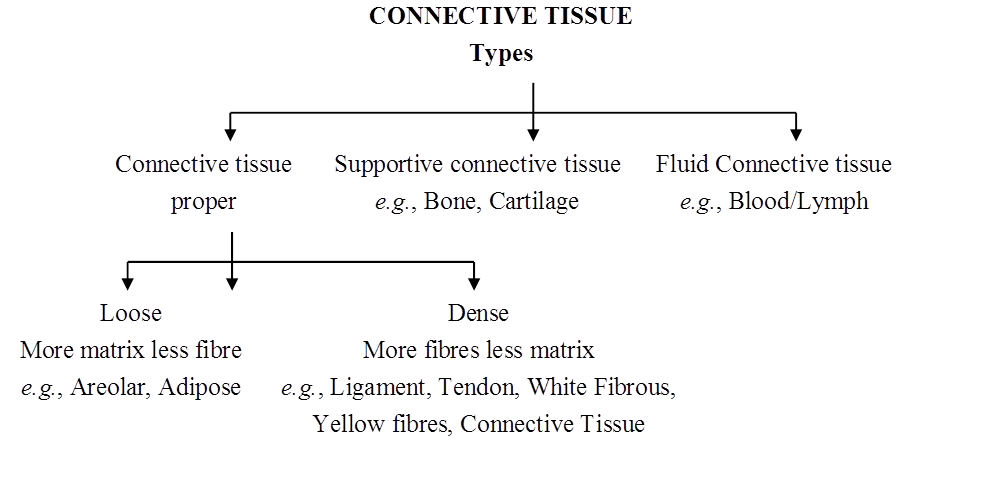
(1) Connective Tissue Proper
(I) Loose Connective Tissue:
It consists of cells scattered within an amorphous mass of proteins that forms a ground substance.
The gelatinous material is strengthened by a loose scattering of protein fibres such as collagen, elastin, which makes tissue elastic and reticulin, which supports the tissue by forming a meshwork.
(a) Adipose Tissue:
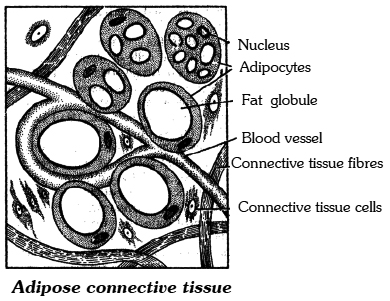
Adipose tissue is a connective tissue rich beneath the skin, around kidneys in mesentery and bone marrow.
Besides fibroblasts, macrophages, collagen fibres and elastic fibres, the adipose tissue also contains large, spherical or oval cells called Fat Cells or Adipocytes.
The cytoplasm and organelles in adipocytes are pressed by fat globule into a narrow annular layer just beneath the plasma membrane.
The adipose tissue synthesises, stores and metabolises fat.
Functions:
(i) Preventing heat loss by forming heat-insulating layer beneath the skin.
(ii) Forming shock-absorbing cushions around kidneys and eyeballs.
(iii) Acting as a food reserve.
White and Brown Tissue:
The cells of adipose tissue are characterized by droplets of fats in the cytoplasm of connective tissue cells.
There are two kinds of fatty tissues. In the white adipose tissue, there is a single large fat droplet in the cells surrounded by a small amount of the cytoplasm.
The brown adipose tissue-cell on the other hand has many small droplets of fat, suspended in a considerably larger amount of cytoplasm.
Whereas brown fat cells contain many mitochondria, the white fat cells have comparatively few.
The colour in the brown fat is due to a high concentration of iron-containing cytochrome pigments.
Brown fat is particularly found in new-born babies and hibernating mammals.
It accounts for 5-6 percent of the body weight of the new-born rabbit and also of man.
Brown fat has a larger capacity for generating heat.
It is because of brown fat that new-born mammals generally do not shiver inspite of lower temperature outside.
Brown fat cannot be a substitute of food. Adipose tissue may be examined from the fat bodies of frog or from the skin of rabbit.
(b) AreolarTissue:
It occurs beneath the epithelia of many hollow visceral organs, skin and in the walls of arteries and veins. The areolar tissue contains different types of cells.
(i) Fibroblasts are the principal cells of this tissue. They are irregularly-shaped flat cells with long protoplasmic processes. Fibroblasts synthesise two kinds of protein-collagen and elastin. Fibroblast secrete the major amount of matrix.
(ii) Macrophage / Histiocytes / Clasmatocytes: They are phagocytic in nature.
(iii) Mast cells / Mastocytes: They are irregular or ovoid cells and contain basophilic granules which are made of:
Histamine - Inflammatory substance produced during allergic reactions.
Heparin - Natural anti-coagulant.
Serotonin - Vasoconstrictor.
(iv) Plasma cells / cart wheel cells synthesise antibodies.
The areolar tissue joins different tissues and forms the packing between them and helps to keep the organs in place and in normal shape.
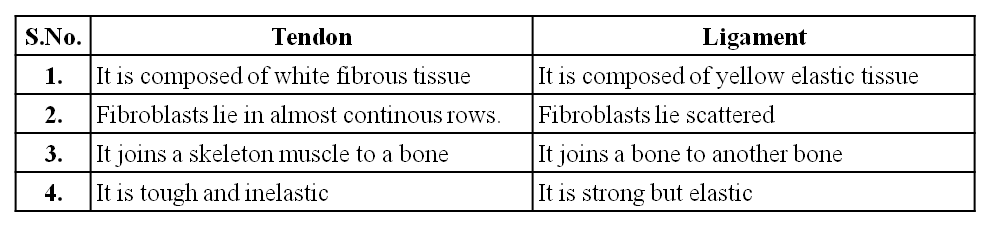
(II) Dense Connective Tissue:
Fibres and fibroblasts are compactly packed in the dense connective tissues.
Orientation of fibres show a regular or irregular pattern and are called dense regular and dense irregular tissues.
In the dense regular connective tissues, the collagen fibres are present in rows between many parallel bundles of fibres e.g. tendons and ligaments.
Dense irregular connective tissue has fibroblasts and many fibres (mostly collagen) that are oriented in different directions.
This tissue is present in the skin, perimysium, perineurium and around bones as periosteum.
(a) White Fibrous Tissue:
It carries only a few fibroblasts scattered amidst the dense network of thick collagen fibre bundles. It has great tensile strength. The presence of white fibrous tissue at the joints between skull bones makes them immovable.
(b) Tendon:
It is a very dense, strong and fibrous connective tissue with thick parallel bundles of collagen fibres. A few flat, elongated tendon cells lie in a single rows between the fibre bundles. Tendon forms the strong inextensible attachment of a skeletal muscle to a bone. Colloidal protein gelatin is obtained by boiling collagen.
(c) Ligament:
Ligaments connect the bones at the joints and hold them in position. Sprain is caused by excessive pulling of ligaments. They are made of bundles of elastic fibres and few collagen fibres. Many year old mummies still have their arteries intact due to well preserved elastic fibres.
Difference between Tendon and Ligament
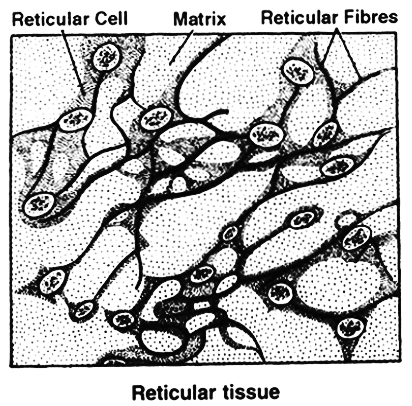
(d) Reticular tissue:
It consists of star-shaped reticular cells whose protoplasmic processes form a network. These cells are phagocytic in function. Matrix and some other types of cells are also found in the spaces of the network. Reticular tissue is present in the spleen, lymph nodes, bone marrow, etc.
(2) SUPPORTIVE CONNECTIVE TISSUE
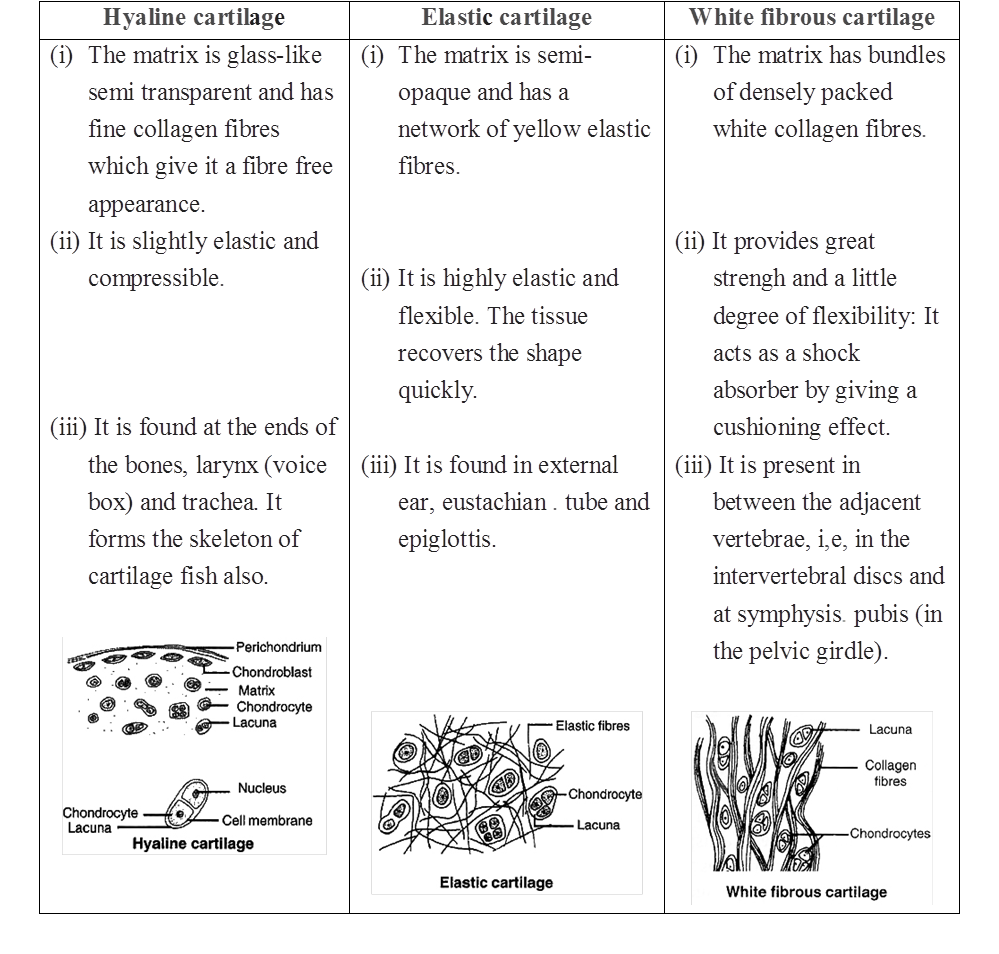
(I) Cartilage:
Cartilage is a solid but semi-rigid and flexible connective tissue. Chondrocytes are large, blunt, angular cartilage cells.
They occur in clusters of 2 or 3 cells in small spaces (lacunae) scattered in the matrix.
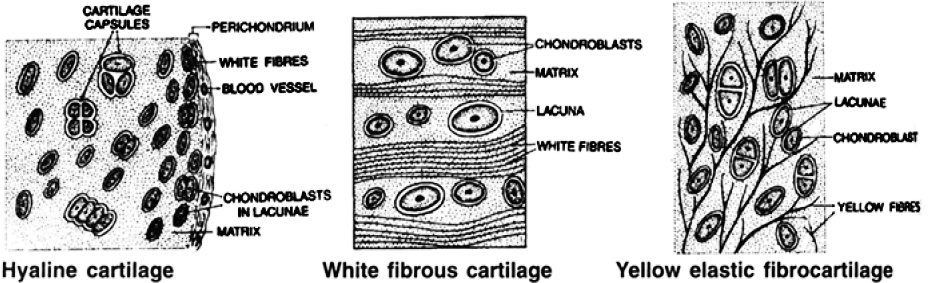
(a) In Hyaline Cartilage, the matrix is apparently fibre-less and glass-like (hyaline) but translucent. It occurs in the larynx, nasal septum, tracheal rings and costal cartilage, It gives those structures a definite but pliable form. White Fibrocartilage carries thick dense bundles of collagen fibres between rows of chondrocytes in lacunae. It occurs in joints between vertebrae. Its collagen fibres make such joints strong but less elastic and only slightly movable.
Nucleus Pulposus - In the centre of the intervertebral disc, a soft area is present called nucleus pulposus which is supposed to be a remnant of notochord.
(b) Elastic Cartilage contains a dense network of elastic fibres between scattered chondrocytes. It forms the eustachian tube, epiglottis and pinna of ear. The elastic fibres make those organs considerably elastic and pliable.
(c) Calcified Cartilage -Initially it is like hyaline cartilage but later on it gets hardened like bone due to deposition of calcium salts, e.g., supra scapula of frog's pectoral girdle, pubis of pelvic girdle of frog.
Table : Types of Cartilage
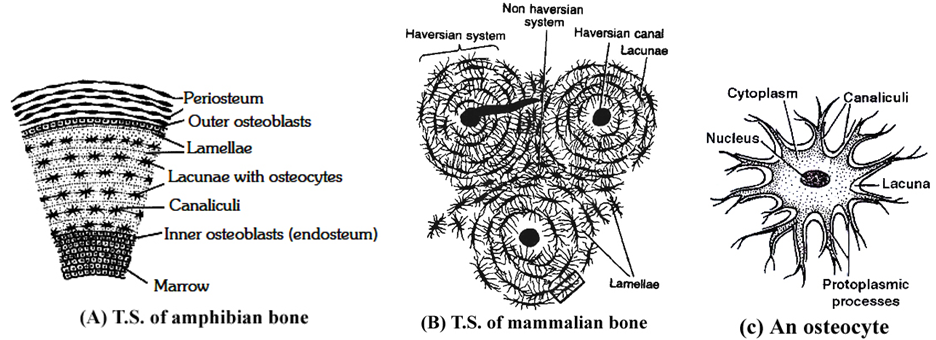
(II) BONE
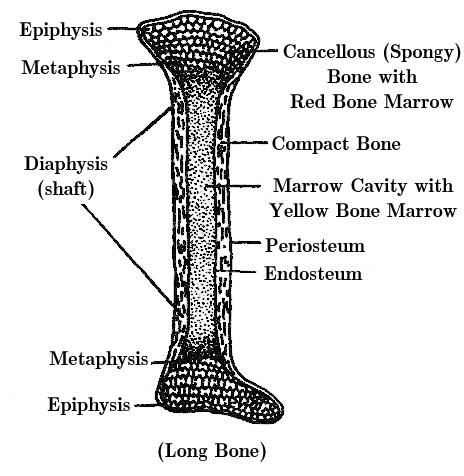
(i) It is a solid, rigid connective tissue. The matrix of the bone has the deposition of apatite salts of calcium and phosphorus. e.g, hydroxyapatite salts and fluoroapatite salts.
(ii) 60-70% of bone is made up of inorganic matter and 30-40% is made up of organic matter.
(iii) If the bone is put in dil. HCl, the bone becomes decalcified, soft and flexible. Nothing will happen to bone if we put the bone in KOH.
(iv) Osteoblast are bone forming cells which secrete ossein protein.
(v) Osteocytes are bone cells, they are metabolically inactive cells present in lacuna.
(vi) Bone is a solid, rigid and strong connective tissue. Its matrix is heavily deposited with apatite salts of calcium and phosphorus. Flat irregular spaces called Lacunae occur in the solid matrix. Each lacuna lodges a flat bone cell or Osteocyte. A bone cell has an irregular shape and long cytoplasmic processes. These processes extend into minute canals (Canaliculi) radiating from each lacuna.
(vii) Compact Bone forms the dense outer layers of all bones. It is composed of many parallel, longitudinal, column-like structures called Haversian Systems, cemented to each other. Haversian canals are connected to each other by Volksman canals. In each Haversian system, several concentric layers (Lamellae) of bony matrix encircle a longitudinal central canal (Haversian Canal). This canal carries blood vessels and nerves. Lacunae containing osteocytes occur in a layer between two lamellae.
(viii) Spongy Bone -The ends of long bones are composed of an open lattice of bone called spongy bone. The spaces within contain marrow, where most blood cells are formed. It carries no concentric organisation like the Haversian system. It consists of a network of many fine irregular bony plates or Trabeculae. Each trabecula consists of many irregularly arranged lamellae with lacunae between them. It has red bone marrow. Spongy bone is also called as cancelfous bone and is found in epiphysis, i.e., the ends of long bones.
Table : Differences between bone and cartilage
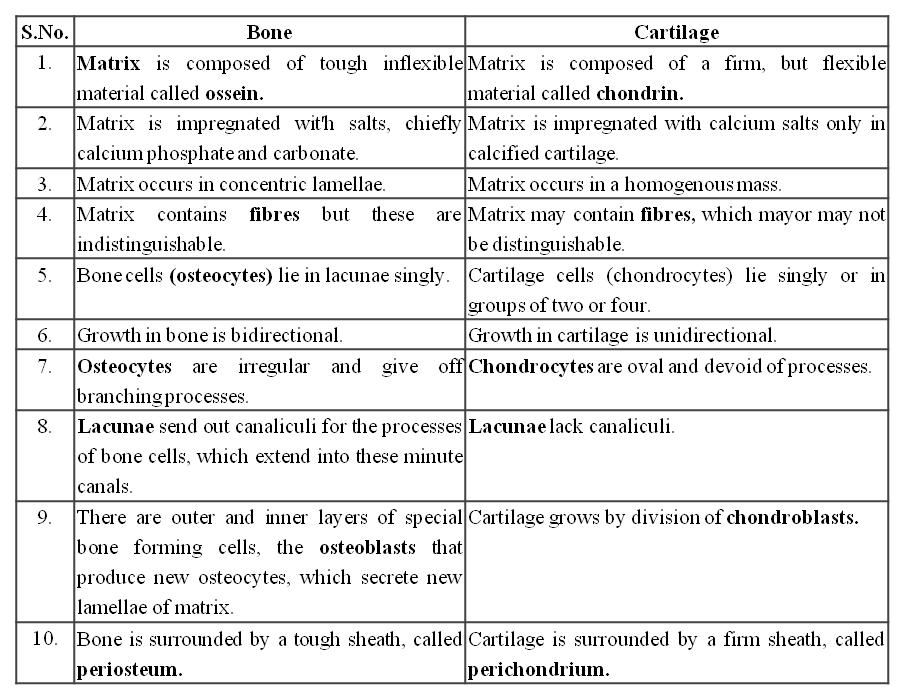
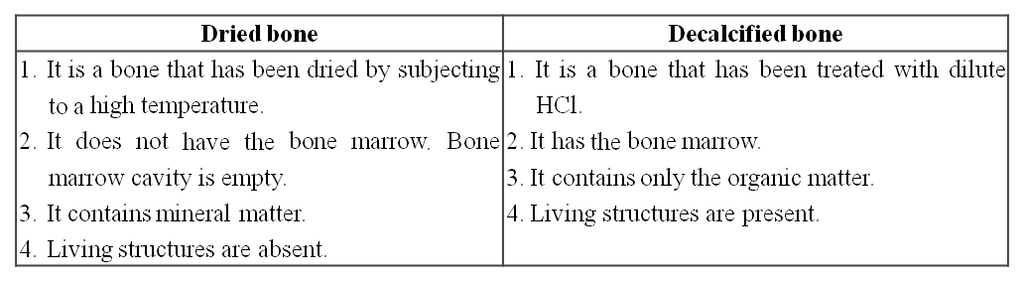
Table : Differences between a Dried bone and a Decalcified bone
Concept Builder
Types of Bones :
(i) Cartilage bones / Endochondrial / Replacing bones - They are formed by the replacement of cartilage by the bone e.g. humerus, femur, vertebrae, ribs, girdle bones except clavicle. Chondroclasts are cartilage eater cells.
(ii) Membrane / Investing bone / Dermal - e.g. skull bones, clavicle. The bones are formed in the dermis of the skin and are invested over the already present cartilages.
(iii) Sesamoid bones - They are formed by the ossification of the tendons e.g., Patella.
(iv) Visceral bones - They are those bones which get detached from the skeleton and come to lie in visceral organs e.g.,
(a) os cordis - Present in interventricular septum of heart of deer.
(b) os falciparum - Palm of mole.
(c) os penis - Penis of rat and carnivores.
(d) os palbebrae - In the eyelids of crocodile.
(e) os rostralis - Snout of pig.
1. Bone China: Porcelain was first made in China during tang dynasty. English found a new way of making porcelain with bone ash. Bone china is a form of porcelain made from burned animal bones. Bone ash is mixed with kaolin, a white clay. The bone ash increases the porcelain's translucence.
2. Word Roots and Origins : Periosteum from the Greek "peri" meaning "around" and "osteon" meaning bone.
(3) FLUID CONNECTIVE TISSUE
BLOOD
Blood is a fluid connective tissue.
Its cells are quite distinct from other connective tissue cells both in structure and functions.
The extracellular material in blood is a fluid devoid of fibres.
Fluids outside the cells are generally called Extracellular Fluids (ECF).
Blood is heavier than water.
The extracellular material in blood is a straw-coloured, slightly alkaline (pH =7.4) aqueous fluid called plasma.
Constituents, having characteristic forms, float in the plasma.
They are collectively called the Formed Elements of blood.
They include the blood cells and blood platelets.
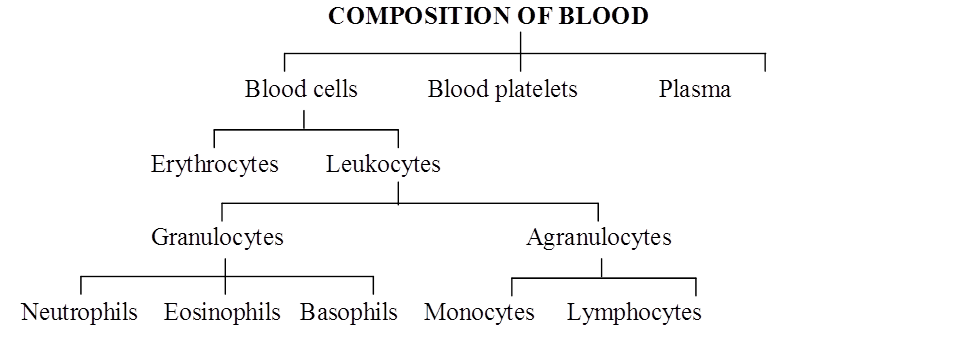
Blood cells are of two types-Erythrocytes and Leukocytes.
Blood circulates within blood vessels in higher animals.
But other extracellular fluids such as cerebrospinal fluid, interstitial fluid, lymph and aqueous humour occur outside blood vessels.
COMPOSITION OF BLOOD
PLASMA
Plasma contains three major classes of plasma proteins viz. serum albumin, serum globulins and fibrinogen.
Plasma proteins serve as a source of proteins for tissue cells.
Tissue cells may utilise plasma proteins for forming their cellular proteins.
Additionally, albumin and globulins retain water in blood plasma by their osmotic effects.
A fall in plasma proteins leads to movement of excessive volumes of water from blood to tissues.
That is why hands and feet get swollen with accumulated fluid (oedema) in persons suffering from dietary deficiency of proteins.
Albumins and globulins also transport many substances such as thyroxine and Fe3+ in combination with them.
One class of globulins, called immunoglobulins, act as Antibodies.
Plasma proteins also maintain the blood pH by neutralising strong acids and bases.
Thus, they act as Acid-Base-Buffers.
It is slightly alkaline non-living inter-cellular substance which constitutes about 60% part of the blood.
It is a pale yellow but transparent and clear fluid.
Composition of Plasma. Plasma forms 55-60% by volume of blood.
1. Water-Water alone forms about 90% to 92% of the plasma. Solids form about 8% of the plasma.
2. Mineral Salts -These are chlorides, bicarbonates, sulphates and phosphates of sodium, potassium, calcium, iron and magnesium. All salts constitute about 0.9% of plasma. Buffer of the blood is sodium bicarbonate.
3. Nutrients - These include glucose, fatty acids, phospholipids, cho'lesterol, fats, aminoacids, nucleosides, etc. Mineral salts have been mentioned above.
4. Plasma proteins -They constitute about 7 to 8% of plasma. These mainly include albumin 4.4% , globulin 1.5 to 2%, prothrombin and fibrinogen both 0.3%.
5. Defence proteins - Immunoglobulins which act as antibodies and some other substances, such as lysozyme and properdin (a large protein) are always found in the plasma. They destroy bacteria, viruses and toxic substances that may enter into the blood from outside.
6. Excretory substances - These include ammonia, urea, uric acid, creatinine, etc.
7. Dissolved gases - Water of blood plasma contains oxygen, carbon dioxide and nitrogen in dissolved form.
8. Anticoagulant - Blood plasma contains a conjugated polysaccharide, heparin which prevents coagulation of blood inside blood vessels.
9. Hormones - These are secreted and released in blood by endocrine glands.
10. Vitamins and Enzymes-Different kinds of vitamins and enzymes are present in the blood plasma.
Functions of Blood plasma-
These can be summarised as under (i) transport, (ii) retention of fluid in blood, (iii) maintenance of blood pH, (iv) body immunity, (v) prevention of blood loss, (vi) conducting heat to skin for dissipation and (vii) uniform distribution of heat all over the body.
Blood Glucose
Glucose is mainly absorbed in the small intestine.
Glucose is also absorbed in the stomach.
After absorption glucose reaches the blood.
Excess of glucose is converted into glycogen by insulin hormone in the liver and muscles.
Whenever it is required, glycogen is changed back into glucose by glucagon hormone.
Usually blood glucose level is about 80-100 mg per 100 ml of blood, 12 hours after a normal meal.
But its concentration rises soon after a carbohydrate rich diet.
If blood glucose level exceeds 180 mg per 100 ml, it starts appearing in urine.
This condition is called glucosuria.
Fasting glucose is 70 -110 mg/dl. Glucose PP[1] is 110 -140 mg/dl.
If it is higher, it causes diabetes mellitus (hyperglycemia).
If it is less, it causes hypoglycemia (less amount of glucose in blood).
Blood Cholesterol
Usually cholesterol is considered a harmful substance. But it is quite useful in limited amount.
Cholesterol is used in the synthesis of biomembranes, vitamin D, bile salts and steroid hormones.
Its normal amount is 80 -180 mg in 100 ml of blood plasma.
Cholesterol comes in the blood plasma either by intestinal absorption of fats or by the synthesis from the liver or by both.
Saturated fats such as ghee and butter increase cholesterol level in the blood.
Increased blood cholesterol may lead to its deposition in the internal wall of the blood vessels like arteries and veins which causes high blood pressure and heart problems.
Functions of Plasma Proteins
1. Prevention of blood loss - Fibrinogen and prothrombin playa role in blood clotting.
2. Retention of fluid in the blood - Albumin helps in osmotic balance.
3. Body immunity - Certain globulins called immunoglobulins (glycoproteins) act as antibodies in blood and tissue fluid. Antibodies belong to a class of proteins called as immunoglobulins.
4. Maintenance of pH - Plasma proteins serve as acid-base buffers. It means they maintain pH of the blood by neutralizing acids and bases.
5. Transport of certain materials - Thyroxine (hormone) is bound to albumin or specific globulin for transport in the plasma.
6. Distribution of heat - Plasma proteins help in uniform distribution of heat all over the body.
7. Enzymes - Some proteins acting as enzymes also occur in the plasma.
BLOOD CELLS
(i) Erythrocytes:
Erythrocytes (red blood corpuscles or RBC) are the most numerous of the formed elements of blood.
Their most important characteristic feature is the presence of hemoglobin, the red oxygen carrying pigment.
The total number of erythrocytes per microlitre (1 µl = 1mm3 =10–6) of blood is known as the Total Count of RBC.
It averages 5 millions and 4.5 millions in adult man and adult woman respectively.
The total count would be low in anaemia and after profuse bleeding.
On the contrary, the abnormal rise in the total count of RBC is called Polycythemia.
Anaemia is caused due to the deficiency of folic acid, vitamin B12 and haemoglobin.
The size and shape of erythrocytes vary in different classes of animals.
In fishes, amphibians, reptiles and birds, erythrocytes are usually nucleated, oval and biconvex. But in mammals they are non nucleated, biconcave and circular.
Only camel and llama possess oval red blood corpuscles.
Human erythrocytes measure 7-8 µm (1µm =10–6 m) in diameter and 2 µm thickness near the rim.
Old and damaged erythrocytes are phagocytosed and destroyed by macrophages.
The pigment part (porphyrin) of hemoglobin is then catabolised to the yellow pigment Bilirubin which is excreted in the bile.
The pale yellow colour of plasma is largely due to bilirubin.
If a sample of blood is rendered non-coagulable by adding potassium or sodium oxalate and then centrifuged at a high speed in a graduated centrifuge tube (hematocrit tube), the centrifugal force rapidly sediments the erythrocytes tothe bottom of the tube.
They become packed into a solid, red, bottom layer while plasma forms a clear, fiuid upper layer.
On the upper surface of the erythrocyte layer, leukocytes form a thin, buff-coloured layer.
From the graduations on the tube, the relative volume of erythrocytes may be read as a percentage of the total blood volume. This is called the Hematocrit Value or Packed Cell Volume.
It normally forms 45 percent of the blood volume.
RBC of mammals are circular, biconcave, non-nucleated except family camelidae. e.g. camel, which has non-nucleated and oval RBC. Largest RBCs are found in amphibia.
Smallest RBCs are found in mammals.
In mammals smallest RBCs are found in 'Musk Deer', Tragulus javanicus (1.5 µm).
In mammals, largest RBCs are found in elephant. (9.4 µJ).
Graveyard of RBC is spleen.
Life Span
Life span of RBC in man =120 days
Life span of RBC in frog = 100 days
Life span of RBC of rabbit = 80 days
Radioactive chromium method (Cr51) is used for estimation of life span of RBC.
Count of RBC
In embryo = 8.5 million/mm3
In Man = 5 to 5.5 million/mm3
In Woman = 4.5 million/mm3
Daily destruction of RBC = 1%
ESR (Erythrocyte sedimentation rate) : It is measured by Wintrobe's method. It is rate of settling down of RBC.
It is also estimated by Westergen's method.
ESR is very useful in diagnosing various diseases including tuberculosis, ESR in men is 0-5 mm/hour and in women it is 0-7 mm/hr in Westergen method.
Haemocytometer : It is instrument for counting the number of both WBCs and RBCs.
Rouleaux: In resting and slow flowing blood, the RBCs aggregate to form rouleaux (the RBCs are piled on top of each other). Fibrinogen favours rouleaux formation.
Bone marrow : It is the main site for formation of RBC. Volume of bone marrow at the time of birth is 70 ml. In adult volume of bone marrow is 4,000 ml.
Structure of RBC of man : Biconcave non-nucleated bounded by Donnan's membrane (plasma membrane of RBC). Haemoglobin is filled in RBC which is respiratory pigment.
Normal Range of Hb
Infants 16.5 ± 3.0 g/dl (dl = deciliter)
Children 3 months 11.0 ± 1.5 g/dl
Children 3 to 6 years 12.0 ± 1.0 g/dl
Children 10 to 12 years 13.0 ± 1.5 g/dl
Men 15.5 ± 2.5 g/dl
Women 14.0 ± 2.5 g/dl
Structure of Haemoglobin :
Each molecule of haemoglobin contains 4 molecules of haem and 1 molecule of globin.
These are attached by co-ordinate bonds.
Haem is protoporphyrin compound and has 4 pyrrole groups jointed together to form ring structure.
In Hb, Fe is present in (Fe++) Ferrous form.
Haem is 5% & Globin is 95%. Globin is made of 4 polypeptide chains.
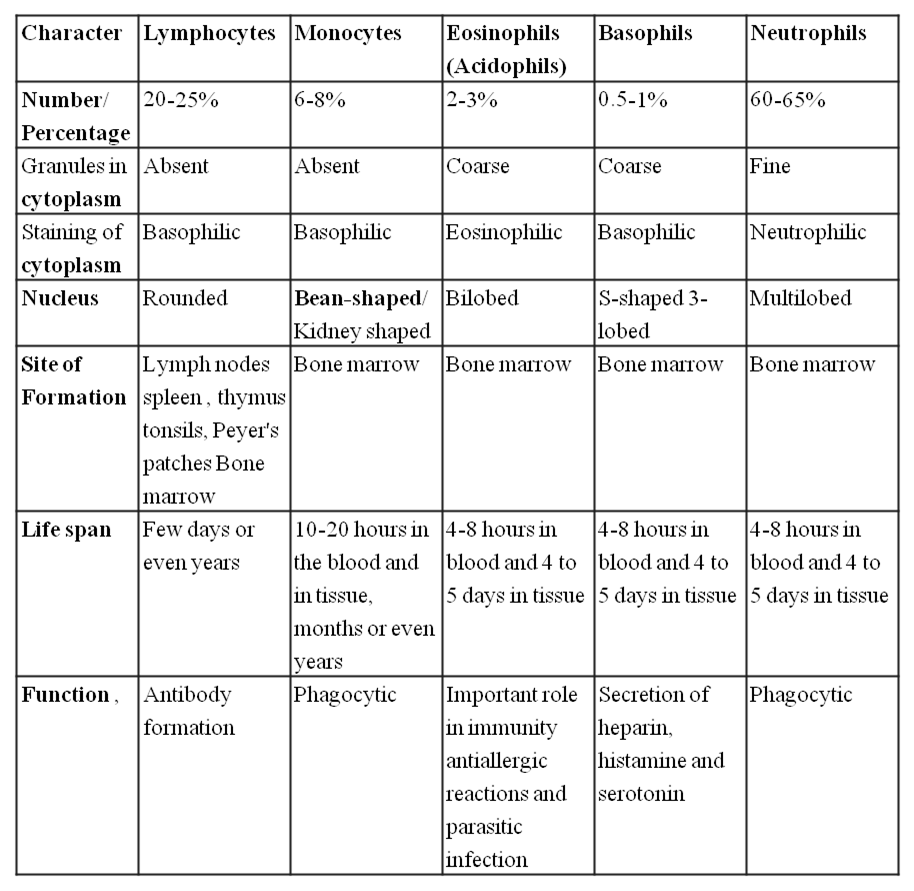
(ii) Leukocytes:
Leukocytes (white blood corpuscles or WBC) are devoid of hemoglobin and are consequently colourless.
Leukocytes are nucleated blood cells.
They are of two major classes : granulocytes (with cytoplasmic granules) and agranulocytes (without granules).
Granulocytes are of three types, viz. neutrophils, eosinophils and basophils, each with lobed nucleus.
Agranulocytesare of two types, viz. lymphocytes and monocytes.
Neutrophils and monocytes protect the body against microbes by phagocytosing them.
Lymphocytes secrete antibodies in the blood to destroy microbes and their toxins.
The number of leukocytes per microlitre (1 µl = 1 mm3 = 10–6) of blood is called the Total Count of WBC.
It is 6000-8000/mm3 of blood normally.
It may rise abnormally in acute infections (e.g., pneumonia), inflammations (e.g. appendicitis) and malignancies (e.g., leukemia).
In some conditions such as folic acid deficiency, the total count falls abnormally (leukopenia).
The total count of WBC is also of diagnostic value in many diseases.
Monocytes have kidney shaped nucleus.
The process by which monocytes and neutrophils squeeze out through thin capillary walls is Diapedesis.
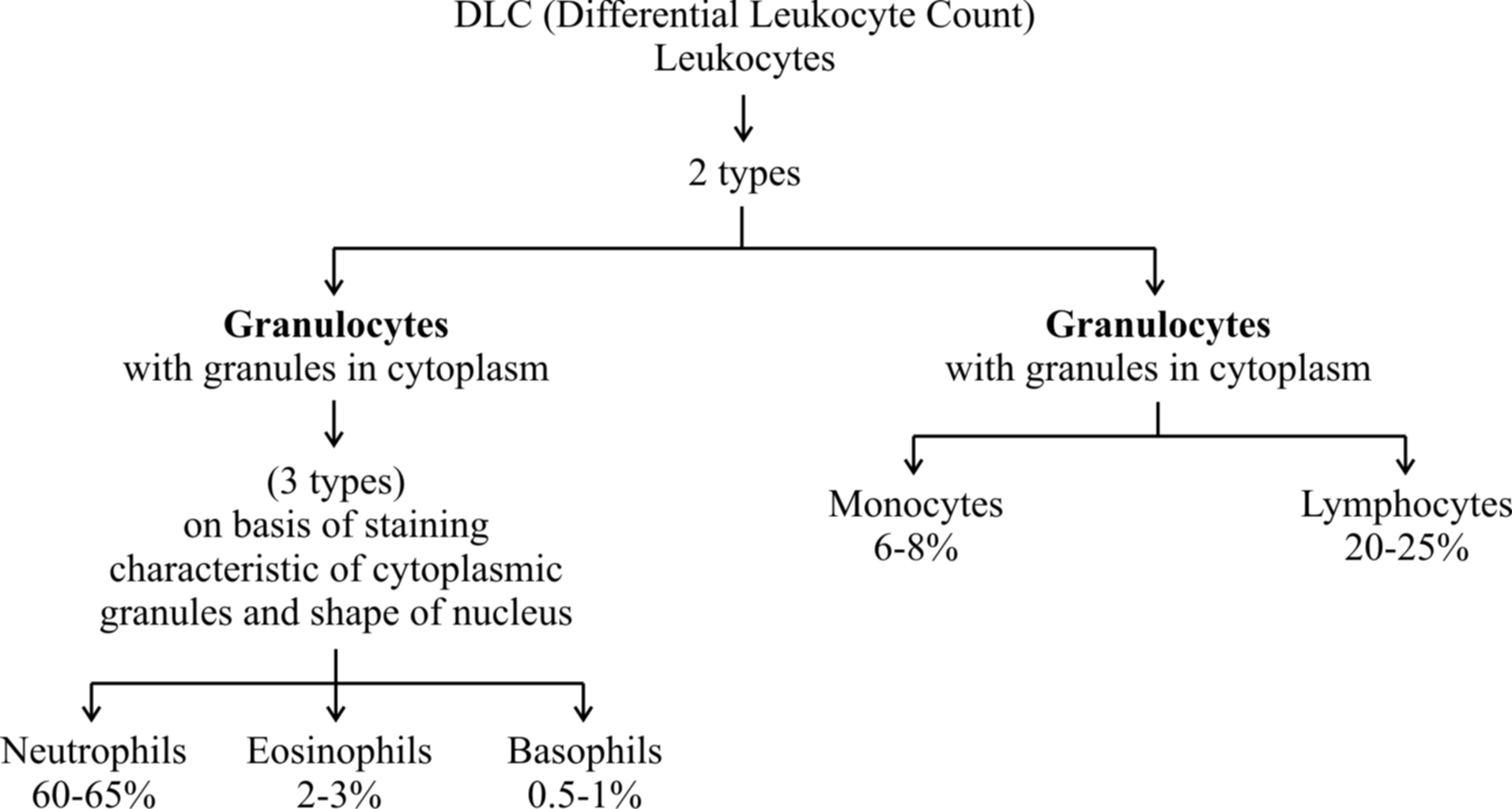
(a) Neutrophils : They are maximum in number, stain equally with both basic and acidic dyes and have many lobed nucleus, granules are in abundance in cytoplasm and help in phagocytosis.
(b) Eosinophils : They have bilobed nucleus, stain with acidic stains. Their number increases during allergic reactions (Eosinophilia).
(c) Basophils: They stain with basic dyes. Their nucleus is 'S' shaped. Coarse granules are few in the cytoplasm. Basophils release heparin and histamine in the blood and have a function similar to the mast cells.
(d) Lymphocytes have large and rounded nucleus. The cytoplasm forms a thin peripheral film. They have their stem cells in the bone marrow and are differentiated in the bone marrow or in the thymus. Lymphocytes are of two types, B-lymphocytes and T-lymphocytes.
B-lymphocytes produce antibodies against antigens and they mature in the bone marrow.
(e) Monocytes are the largest leucocytes (12-15 µm). The nucleus is kidney shaped. They are produced from bone marrow monoblast cells. They help in phagocytosis.
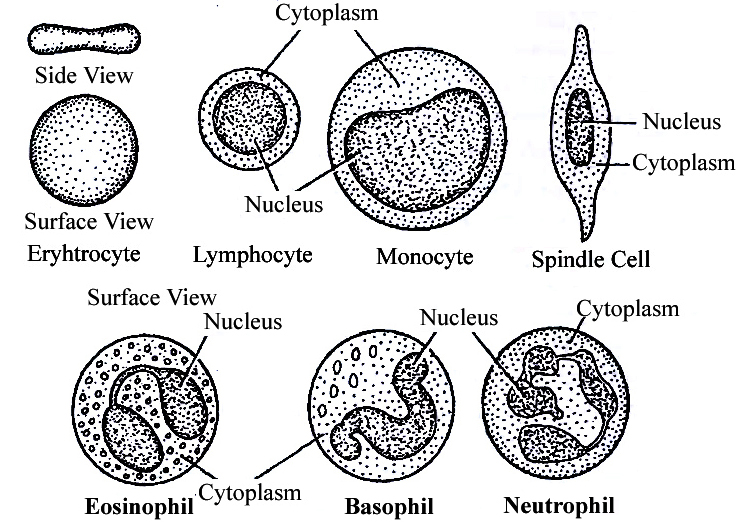
Table : Differences between different types of Leucocytes
(iii) Blood platelets:
Also called thrombocytes, blood platelets are non-nucleated, round or oval, biconvex disc-like bodies.
They are 2-3 micrometres in diameter and their number normally varies from 0.15 to 0.35 million/mm3 or 150000 -350000 platelets/mm3.
They bud off from the cytoplasm of very large Megakaryocytes of the bone marrow.
Their normal life-span is about a week.
When a blood vessel is injured, platelets get clumped at the injured spot and release certain chemicals called Platelet Factors.
These promote blood coagulation.
Thrombocytopenia is decrease in platelet count and Purpura is a group of bleeding diseases due to thrombocytqpenia.
BLOOD COAGULATION
When blood oozes out of a cut, it sets into gel within a few minutes. This is called coagulation.
Coagulation is brought about by hydrolysis of soluble fibrinogen of plasma to insoluble fibrin.
This is catalysed by an enzyme called thrombin.
Fibrin precipitates as a network of fibres.
This network traps many blood cells, particularly RBCs, to form a red solid mass called the Blood Clot.
The clot seals the wound in the vessel to stop the bleeding.
The straw coloured fluid left after clotting of blood, is called Serum.
The serum cannot be coagulated as it lacks fibrinogen.
Thrombin occurs in normal blood as an inactive globulin called Prothrombin.
It must be activated to thrombin before blood coagulation can occur.
In case of injury to a blood vessel, coagulation promoting substances called Thromboplastins are released into the blood from clumped platelets and damaged tissues.
Thromboplastins help in the formation of the enzyme Prothrombinase.
This enzyme hydrolyses prothrombin to thrombin to initiate coagulation.
Ca2+ ions are essential for both activation and action of thrombin.
Blood normally contains an anticoagulant, Heparin which prevents activation of prothrombin, Heparin is released from mast-cell granules.
Blood also contains Antithrombin which inhibits any thrombin formed accidentally.
Blood drawn from a blood vessel can be kept uncoagulated by adding a pinch of oxalate (sodium or potassium oxalate) to it.
Oxalate precipitates Ca2+ and consequently prevents coagulation.
Chilling of blood also delays coagulation because lesser temperature depresses the action of coagulation promoting enzymes.
Concept Builder
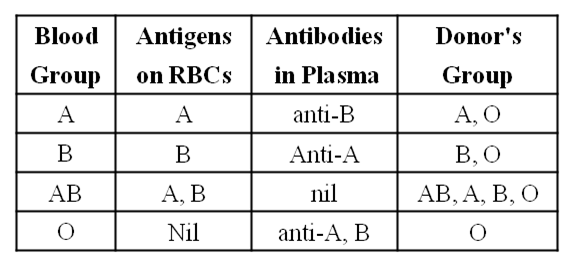
ABO Blood cloting factor :
Karl Landsteiner reported for the first time ABO blood groups in human beings.
A. B and O blood groups were discovered by Landsteiner (1900) while AS blood group was found out by de Castello and Steini (1902).
Agglutinogens (antigens) are present on the surface of red blood corpuscles and agglutinins (antibodies) are found in the blood plasma. Both antigens and antibodies are proteins.
When two different type of blood are mixed, the red blood corpuscles form a clump.
The clumping of red blood corpuscles is called agglutination.
Clotting Factors :
13 factors help in blood clotting.
These factors are mainly produced in liver.
Vitamin K is required in the synthesis of these clotting factors.
These factors are represented in Roman number.
I – Fibrinogen
II – Prothrombin
III – Thromboplastin
IV – Ca+2 (cofactor in each step of blood clotting)
V – Proaccelerin
VI – Accelerin (Rejected)
VII – Proconvertein
VIII – AHG Anti Haemophelic Globin (Absent in Haemophilia-A)
IX – Christmas factor
X – Stuart factor
XI – PTA (Plasma Thormboplastin Anticedent)
XII – Hagman factor
XIII – FSF Factors (Fibrin stabilizing factor) (Laki Lor and factor).
Other natural anticoagulants are
Hirudin – found in leech.
Anophelin – found in female Anophelese.
Lampredin – found in Peteromyzon (Lamprey)
Cumerin – obtain from plants
Warfarin – obtain from plants
To collect blood in bottle in blood bank artificial anticoagulants are used like
Sodium citrate
Sodium oxalate
EDTA (Ethylene diamine tetra acetic acid)
These chemicals act as Calcium binding units and remove Ca+2 ions from blood.
Blood group
Agglutination is due to the interaction of antigens and antibodies.
There are two kinds of antigens that are named A and B.
There are also two kinds of antibodies which are called a and b.
The antigen A and antibody a are incompatible (antagonistic) and cause self clumping and cannot exist together.
Similarly, the antigen B and antibody b are incompatible and cause self clumping and cannot exist together.
Thus, A and b can exist together and B and a can exist together.
The corpuscle factors A and B can occur together if their antagonistic plasma factors a and b are not present.
The plasma factors a and b can occur together if their antagonistic corpuscle factors A and B are absent.
Rh Factor
Another-antigen, the Rh antigen similar to one present in Rhesus monkeys (hence Rh), is also observed on the surface of RBCs of majority (nearly 80 per cent) of humans.
In India % ratio of Rh is
Rh+ – 97%
Rh– – 3%
In World
Rh+ – 80%
Rh– – 20%
Such individuals are called Rh Positive (Rh+ve) and those in whom this antigen is absent are called Rh negative (Rh-ve).
An Rh-ve person, if exposed to Rh+ve blood, will form specific antibodies against the Rh antigens.
Therefore, Rh group should also be matched before transfusions.
A special case of Rh incompatibility (mismatching) has been observed between the Rh-ve blood of a pregnant mother with Rh+ve blood of the foetus.
Rh antigens of the foetus do not get exposed to the Rh-ve blood of the mother in the first pregnancy as the two bloods are well separated by the placenta.
However, during the delivery of the first child, there is a possibility of exposure of the maternal blood to small amounts of the Rh+ve blood from the foetus.
In such cases, the mother starts preparing antibodies against Rh antigen in her blood. In case of her subsequent pregnancies, the Rh antibodies from the mother (Rh-ve) can leak into the blood of the foetus (Rh + ve) and destroy the foetal RBCs.
This could be fatal to the foetus or could cause severe anaemia and jaundice to the baby.
This condition is called erythroblastosis foetalis.
This can be avoided by administering anti-Rh antibodies to the mother immediately after the delivery of the first child
 Maria Habib
Maria Habib
