male reproductive system
- Books Name
- A TEXT OF BIOLOGY - CLASS XII
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 12
- Subject
- Biology
HUMAN REPRODUCTION
Human beings are unisexual.
The growth, maintenance and function of the gonads are regulated by gonadotropins secreted from anterior lobe of pituitary gland.
The organs which neither produce gametes nor secrete sex hormones but perform important functions in reproduction are called secondary sex organs.
The latter include the prostate, seminal vesicles, vas deferentia and penis in males, and the fallopian tubes, uterus, vagina and mammary glands in females.
The characters which distinguish the male from the female externally are called accessory or external sex character. They are also called secondary sex characters.
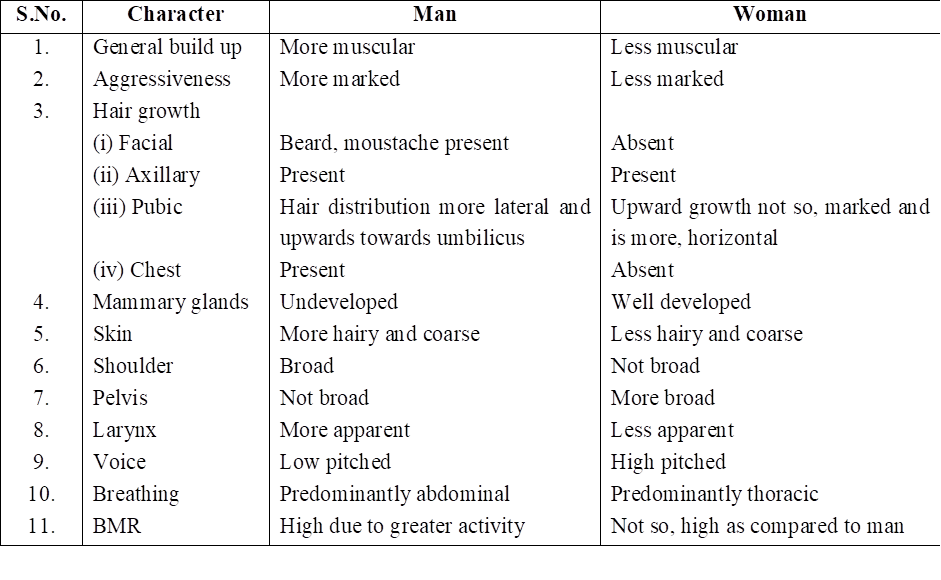
Secondary Sexual Features in Man and Woman
MALE REPRODUCTIVE SYSTEM
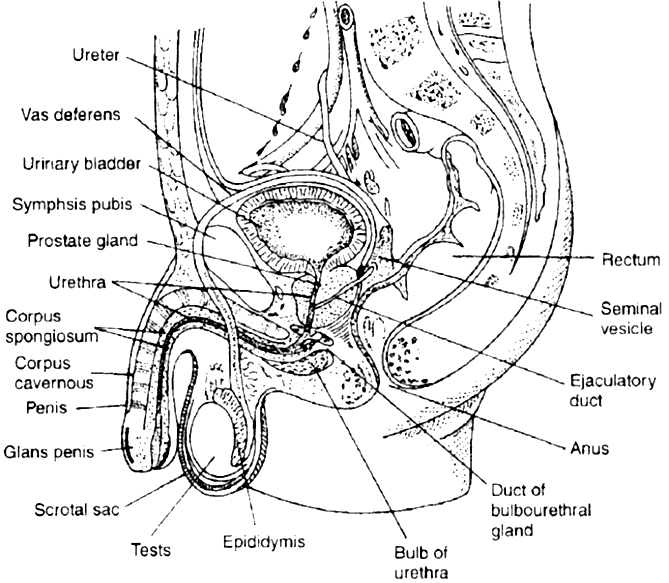
The male reproductive system of mammals consists of a pair of testes, several accessory glands, a duct system and a mating organ called the penis. Testis is the primary male sex organ. It produces spermatozoa and secretes the male sex hormone testosterone.
The human testis measures about 5 cm, 3 cm and 2.5 cm, respectively, in length, thickness and width. It is covered by thick, fibrous, connective tissue called tunica albuginea.
In man, both testes normally remain suspended in a pouch called scrotum outside the abdominal cavity. This keeps the testes at a low temperature than the body temperature (about 2°C below)-this is essential for the maintenance and normal functioning of the spermatogenic tissue of the testes.
Testes descend in the scrotal sac when foetus is about 7 months old and this occurs under the influence of FSH and testosterone.
If testes fail to descend, than the condition is called cryptorchidism that leads to sterility. Scrotum remains connected with the abdomen or pelvic cavity by the inguinal canal. Blood vessels, nerves and conducting tubes pass through inguinal canal.
Cremaster muscles and connective tissue form spermatic cord and surround all structures passing through inguinal canal. Cremaster muscles and dartos muscles of the scrotal sac help in the positioning of testes.
Whenever the outside temperature is low, these contract to move the testes close to the abdominal cavity/pelvic cavity. When outside temperature is high, these relax moving the testes away from the body.
In some seasonally breeding mammals, testes descend into the scrotum during breeding season but ascend back into the abdomen in the non-breeding season. e.g. rats and bats.
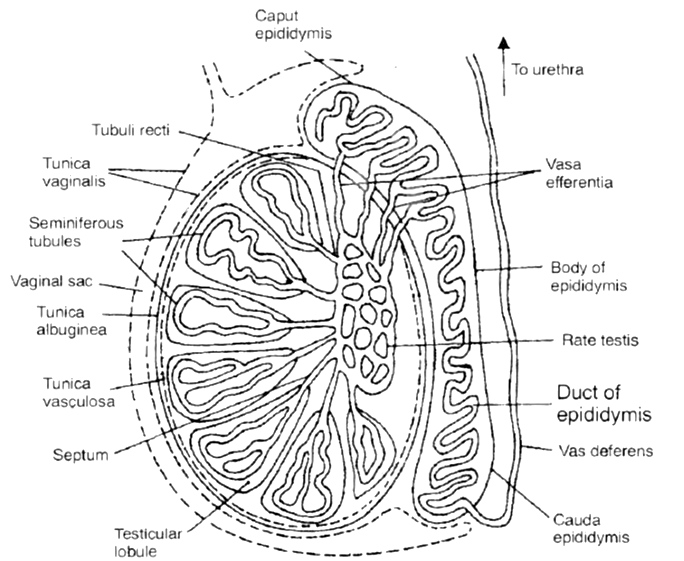
ANATOMY OF TESTIS
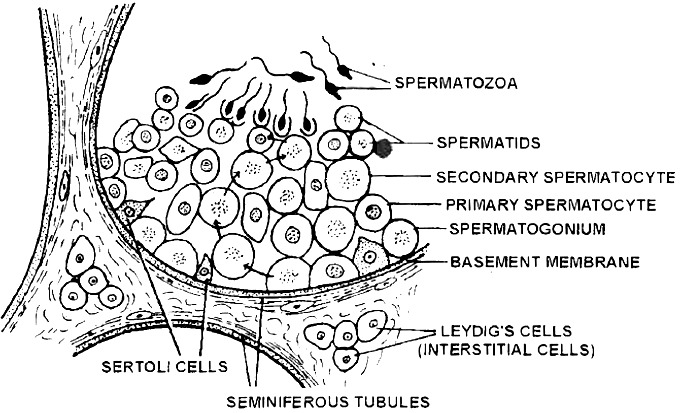
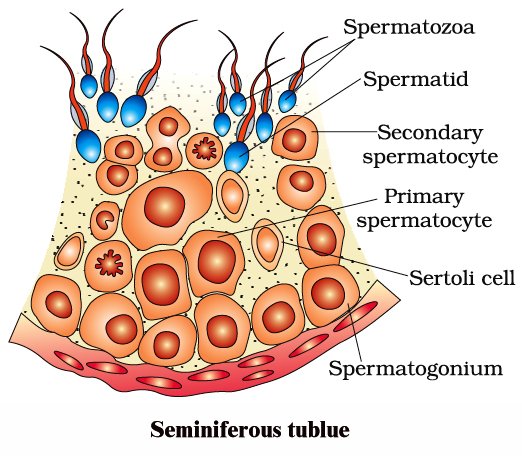
Each testis contains numerous tiny, highly convoluted tubules, called seminiferous tubules. They constitute the spermatogenic tissue of the testis.
Cells lining these tubules give rise to spermatozoa which are released into the lumen of the tubule.
In between spermatogenic cells, Sertoli or sustentacular or nurse cells are present which provide nourishment to the developing spermatozoa and regulate spermatogenesis by releasing inhibin to check FSH overactivity.
The other functions of sertoli cells include
(i) Provide nourishment to the developing spermatozoa,
(ii) Absorb the parts being shed by developing spermatozoa
(iii) Release anti mullerian factor (AMF) to prevent development of mullerian duct/oviduct
(iv) Release of androgen binding protein (ABP).
Groups of polyhedral cells called Interstitial cells or Leydig cells, are located in the connective tissue around the seminiferous tubules.
They constitute the endocrine tissue of the testis. Leydig cells secrete testosterone into the blood.
Seminiferous tubules unite to form several straight tubules called tubuli recti which open into irregular cavities in the posterior part of the testis.
It is highly anastomosing labyrinth of cuboidal epithelium lined channels called rete testis.
Several tubes called vasa efferentia arise from it and conduct spermatozoa out from the testis (Seminiferous tubule to vasa efferentia form intratesticular genital duct system).
The extratesticular duct system consists of tubes which conduct sperms from the testes to the outside.
It starts with vasa efferentia which arise from each testis and becomes confluent to form a folded and coiled tube called epididymis behind each testis.
The epididymis consist of 3 parts: (i) Caput, (ii) Corpus, (iii) Cauda. The epididymis stores the sperms temporarily.
From cauda epididymis, a partially coiled tube called vas deferens ascends into the abdomen through inguinal canal, passes over the urinary bladder, receives the duct from the seminal vesicle behind the urinary bladder to from an ejaculatory duct.
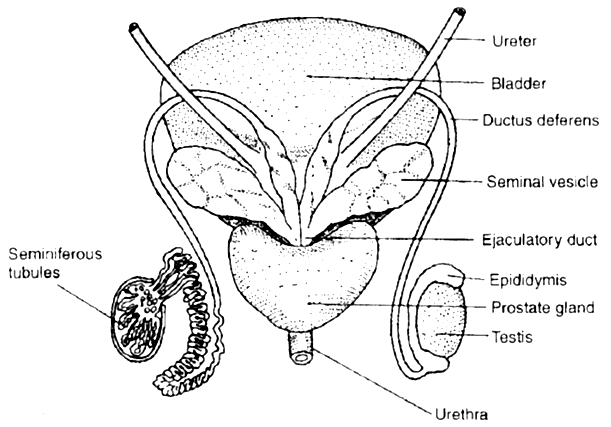
Before entering prostate, the ductus deferens dilates to form ampulla. The final portion of ampulla passes through the prostate to open into the urethra shortly after its origin from the urinary bladder.
The urethra receives the ducts of the prostate and cowper's glands, passes through the penis and opens to the outside.
MALE EXTERNAL GENITAL ORGAN
PENIS
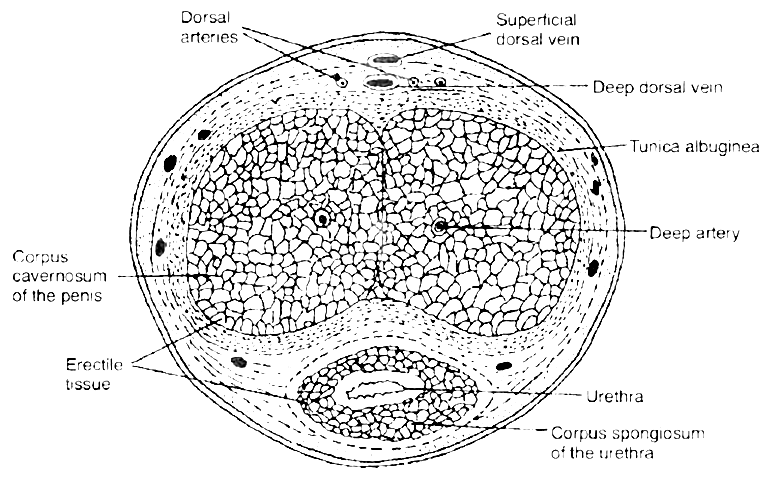
This is the copulatory organ of man. It is a cylindrical and erectile, pendulous organ suspended from pubic region in front of scrotum.
It remains small and limp (= flaccid) but on sexual arousal, it becomes long, hard and erect, ready for copulation (=coitus or intercourse). Erect human penis, on an average is about 15 cm long.
 T.S. of penis
T.S. of penisThe penial mass is itself encased in a fibrous sheath, called tunica albuginea. The interior of penis is mostly formed of three cylindrical cords of spongy, erectile (= cavernous) tissue.
Two of these cords are thicker and situated parallely on right and left sides, forming the thick part of penis that remains in front when penis is limp, but becomes superio-posterior when penis is erect.
These two cords are called corpora cavernosa.
The fibres of tunica albuginea surround both cords jointly and form a separate sheath around each cord. Some fibres form a partition, called septum penis, between these cords.
The third, smaller cord form that part of penis which remains inferio-anterior in erect penis. Urethra runs through this cord. Hence, this cord is called corpus urethrae or spongiosum.
The extended part of corpus spongiosum is enlarged, forming a bulged, conical structure called glans penis. The surface of glans is formed of a thin, smooth and shiny, hairless skin.
The base line of glans is referred to as neck of the penis. The loose skin of penis folds over and is retractile on glans. It is called foreskin or prepuce.
At the tip of glans penis is the slit like external urethral orifice or meatus by which urethra opens out and discharges urine or semen.
Prepucial glands, present in the skin of penis neck, secrete a white sebaceous substance, called smegma. Microbial infection in smegma causes irritation.
GLANDS
Seminal vesicles - These are paired, tubular, coiled glands situated behind the urinary bladder. They secrete viscous fluid which constitute the main part of the ejaculate. Seminal fluid contains fructose, citric acid, inositol and postaglandins.
Prostate gland - It is a chestnut shaped gland and is a collection of 30-40 tubulo-alveolar glands which lies at the base of the bladder and surrounds the base of the urethra. It contributes an alkaline substance to the seminal fluid.
The substance of prostate help the sperms to become active and counteract any adverse effects of urine on sperms. The prostatic fluid provides a characteristic odour to the seminal fluid. Prostate gland secretes -citrate ion, calcium, phosphate ion, and profibrolysin.
Bulbourethral glands or Cowper's glands - The two bulbourethral glands are pea-sized structures lying adjacent to the urethra at the base of penis. These secrete a viscous lubricant.
The duct system, accessory glands and penis are secondary male sex organs. Their growth, maintenance and functions are promoted by testosterone secreted by Leydig cells.
On the other hand, the growth, maintenance and functions of seminiferous tubules and Leydig cells are regulated, respectively by FSH and ICSH of anterior pituitary.
SEMEN
Semen is a mixture of sperms and the secretions of the seminiferous tubules, seminal vesicles, prostate gland, and bulbourethral glands.
The average volume of semen in an ejaculation is 2.5-5 ml, with a sperm count (concentration) of 200 to 300 million. For normal fertility, atleast 60 percent sperms must have normal shape, size and atleast 40 percent of them must show vigorous motility. When the sperm count falls below 20 million/ml, the male is likely to be infertile.
Semen has a slightly alkaline pH of 7.2-7.7. The prostatic secretion gives semen a milky appearance, whereas fluids from the seminal vesicles and bulbourethral glands give it a sticky consistency.
Semen provides transportation medium and nutrients to sperms. It neutralizes the hostile acidic environment of the male urethra and the female vagina.
(Prostatitis - Inflammation of prostate gland.)
female reproductive system
- Books Name
- A TEXT OF BIOLOGY - CLASS XII
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 12
- Subject
- Biology
FEMALE REPRODUCTIVE SYSTEM
The female reproductive system consists of a pair of ovaries, a duct system, consisting of a pair of fallopian tubes (oviduct), an uterus, cervix and vagina. A pair of mammary glands are accessory genital glands.
OVARIES
The ovary is the primary female sex organ. It produces ova and secretes the female sex hormones, estrogen and progesterone that are responsible for the development of secondary female sex characters and regulate cyclic changes in the uterine endometrium.
The human ovaries are small, almond-like flat bodies of about 3 cm in diameter.
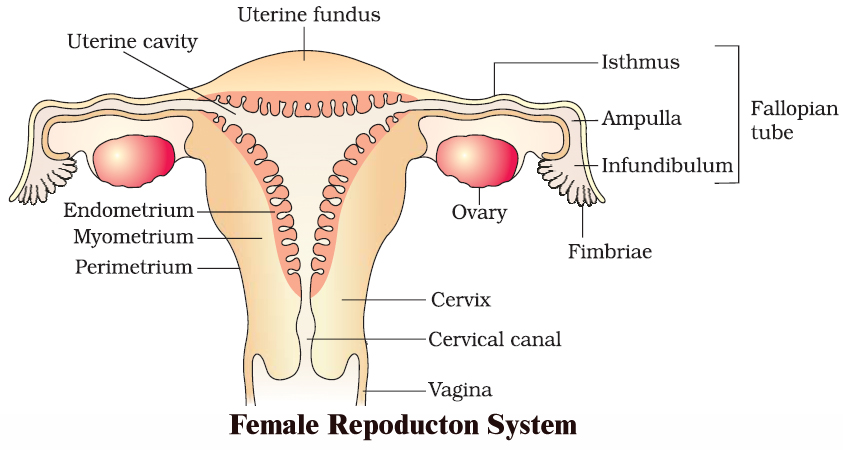
1. Location. Ovaries are located near kidneys and remain attached to the lower abdominal cavity through mesovarium.
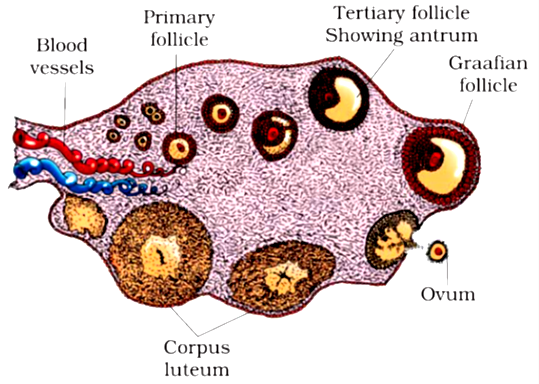
2. Structure. The free surface of the ovary is covered by a germinal epithelium made of a single layer of cubical cells. This epithelium is continuous with the mesothelium, called peritoneum. The epithelium encloses the ovarian stroma. The stroma is divided into two zones-a peripheral cortex and an inner medulla. Cortex is covered by a connective tissue, called tunica albuginea.
The cortex contains numerous spherical or oval, sac-like masses of cells, known as ovarian follicles. The medulla consists of loose connective tissue, elastic fibres, blood vessels and smooth muscle fibres.
 A section of human ovary
A section of human ovaryOVARIAN FOLLICLE
The ovarian follicle carries a large, centrally placed ovum, surrounded by several layers of granular cells (follicular granulosa or discus proligerus or cumulus oophorus). It is suspended in small cavity the antrum.
Antrum is filled with liquid folliculi. The secondary oocyte in the tertiary folicle forms a new membrane called zona pellucida. The follicle bulges on the surface of the ovary.
Such a follicle is called the mature Graafian follicle (after De Graaf, who reported them in 1672).
CORPUS LUTEUM
The ovum is shed from the ovary by rupturing the follicle. The release of ovum is called ovulation and occurs nearly 14 days before the onset of the next menstrual cycle.
After the extrusion of the ovum, Graafian follicle transforms into corpus luteum. Corpus luteum is filled with a yellow pigment, called lutein.
Corpus luteum grows for a few days and if the ovum is fertilized and implantation occurs, then it continues to grow. But if the ovum is not fertilized, then corpus luteum persists only for about 14 days.
It secretes progesterone. At the end of its functional life, the corpus luteum degenerates,and becomes converted to a mass of fibrous tissue, called corpus-albicans (white body) that remains as a scar in the ovary throughout the life of female.
FALLOPIAN TUBES (OVIDUCTS)
There are one pair, long (about 10 cm), ciliated, muscular and tubular structures that extend from ovaries to uterus. Each one is suspended by mesosalpinx. Each fallopian tube is differentiated into four parts :
(i) Infundibulum. The part of oviduct closer to the ovary is the funnel shaped infundibulum. The edges of infundibulum possess finger like projections called fimbriae. Fimbriae help in collection of the ovum after ovulation. Infundibulum opens in abdominal cavity by an aperture called osteum.
(ii) Ampulla. The infundibulum leads to a wider part of the oviduct called ampulla.
(iii) Isthmus. It is middle, narrow and ciliated part of the oviduct.
(iv) Uterine part. It is inner and narrow part which opens in the upper part of uterus.
It is involved in the conduction of ovum or zygote towards the uterus by peristalsis and ciliary action. (Fertilization occurs at the junction of ampulla and isthmus).
Uterus. It is a large hollow, muscular, highly vascular and pear shaped structure present in the pelvis between the bladder and rectum. It is suspended by a mesentery, mesometrium. It is formed of three parts.
(i) Fundus. It is upper dome shaped part above the opening of fallopian tubes.
(ii) Body. It is middle and main part of uterus.
(iii) Cervix. It is lower, narrow part which opens in the body of uterus by internal os and in vagina below by external os. It is formed of most powerful sphincter muscle in the body.
Its wall is formed of outer peritoneal layer called perimetrium; middle muscular myometrium made of smooth muscle fibres, and inner highly vascular and glandular endometrium.
It is the site of foetal growth during pregnancy. It also takes part in placenta formation and helps in pushing the baby out during parturition.
VAGINA
It is a long (7.5 cm), fibro-muscular tube. It extends backward in front of rectum and cervix to the vestibule. It is vascular tube internally lined by mucus membrane and is raised into transverse folds called vaginal rugae.
In the virgin female, vaginal orifice is closed by a membranous diaphragm called hymen which becomes centrally perforated at puberty for the discharge of menstrual flow (or menses).
Vagina acts both as copulation canal as it receives the sperms from penis during copulation and birth canal during parturition.
FEMALE EXTERNAL GENITAL ORGAN
Vulva. It is external genitalia of female. It has a depression, the vestibule, in front of anus. Vestibule has two apertures-upper external urethral orifice of urethra and lower vaginal orifice of vagina.
Mons pubis : Is a fleshy and fatty tissue covered by skin and pubic hair.
Labia majora : It is a pair of fleshy folds which extend from the mons pubis and surround the vaginal opening.
Labia minora : Is another pair of tissue folds below the labia majora.
Both labia majora and labia minora are provided with sebaceous glands.
Hymen : Is a membrane that partially covers the vaginal opening. It gets torn during the first coitus.
Clitoris : Is a tiny, erectile, finger-like structure present at the upper junction of the two labia minora above the urethral opening. The fold of skin that covers clitoris is called prepuce. Clitoris is homologous to penis (as both are supported by corpora cavernosa).
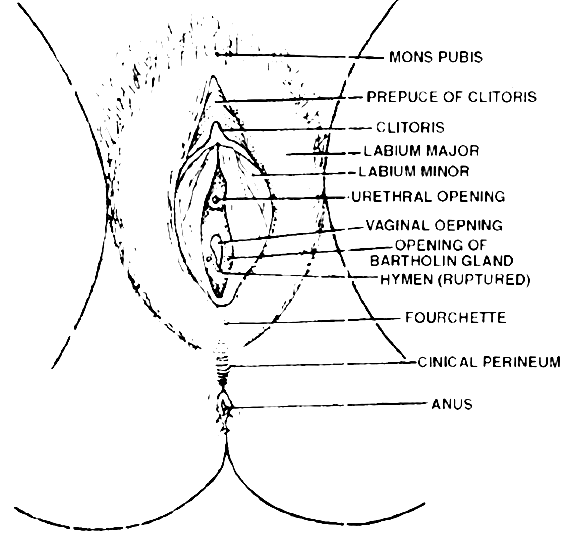
 The external genitalia in the female
The external genitalia in the femaleGLANDS
Vestibular Glands: These are of two types-greater and lesser. Greater vestibular or Bartholin's glands are a pair of small reddish yellow glands on each side of vaginal orifice and secrete alkaline secretion for lubrication and neutralising urinary acidity.
Lesser vestibular glands or paraurethral or skene's glands are small mucus glands present between urethral and vaginal orifices.
MAMMARY GLAND :
Each mammary gland consists of 15-25 lobules of the compound tubuloalveolar type. These lobules secrete milk to nourish the newborn babies.
Each lobe is separated from the others by dense connective and adipose tissue and represents a gland. From each lobe, excretory lactiferous ducts emerge independently in the nipple, which has 15-25 openings, each about 0.5 mm in diameter.
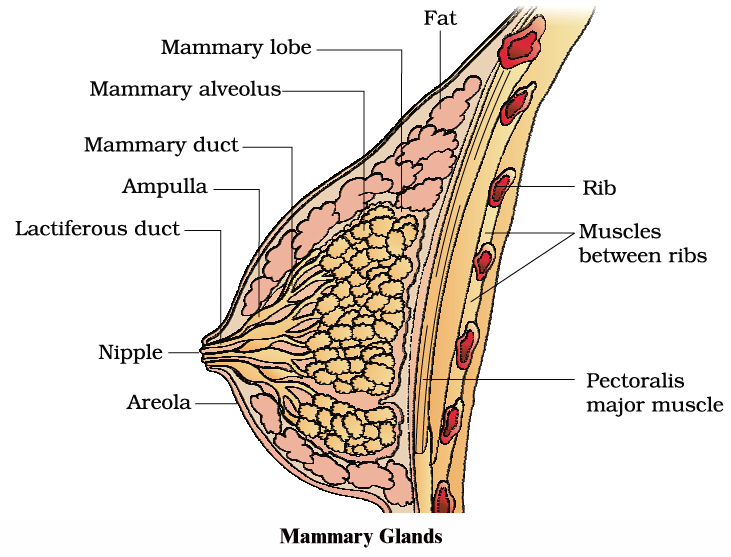
However, the histological structure of mammary glands vary, depending on sex, age and physiological state.
Path of milk ejection :
Mammary alveolus ® Mammary duct ® Ampulla ® Lactiferous duct ® Nipple
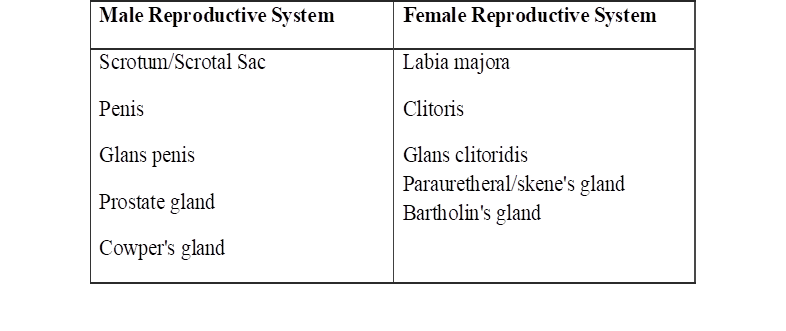
Homology Between Male and Female Reproductive System
gametogenesis
- Books Name
- A TEXT OF BIOLOGY - CLASS XII
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 12
- Subject
- Biology
THE EVENTS IN HUMAN REPRODUCTION
Gametogenesis Insemination Fertilization Implantation Gestation Parturition
FORMATION OF GAMETES
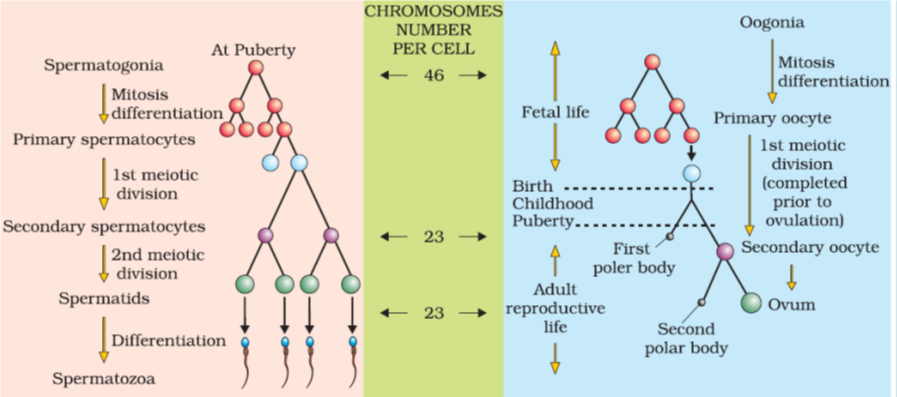
Sexual reproduction requires the fusion of two haploid gametes to form a diploid individual. These haploid cells are produced through gametogenesis.
As there are two types of gametes, the spermatozoa and ova, gametogenesis can be studied under two broad headings: spermatogenesis and oogenesis.
Spermatogenesis is the formation of spermatozoa, whereas oogenesis is the formation of ova. Both spermatozoa and ova originate from primordial germ cells or PGCs, which are extra-gonadal in origin.
In humans, the PGCs originate during early embryonic development from the extra-embryonic mesoderm. Eventually, they migrate to the yolk sac endoderm, and ultimately, to the gonads of the developing embryo, where they undergo further development.
SPERMATOGENESIS
Spermatozoa are produced in the seminiferous tubules of the testes. Spermatogenesis is the process of maturation of reproductive cells in the testes.
Spermatogenesis includes two stages (i) formation of spermatids and (ii) metamorphosis of spermatids. Spermatids are formed by three phases namely phase of multiplication (mitosis), phase of growth and phase of maturation (meiosis).
During phase of multiplication, the primordial germ cells divide repeatedly by mitosis to form diploid spermatogonia.
During phase of growth, the spermatogonium enlarges in size to form primary spermatocyte and prepares to undergo maturation division.
During phase of maturation, the primary spermatocyte undergoes meiosis I giving rise to two haploid (n) secondary spermatocytes. The secondary spermatocytes undergo meiosis II resulting in the formation of four spermatids.
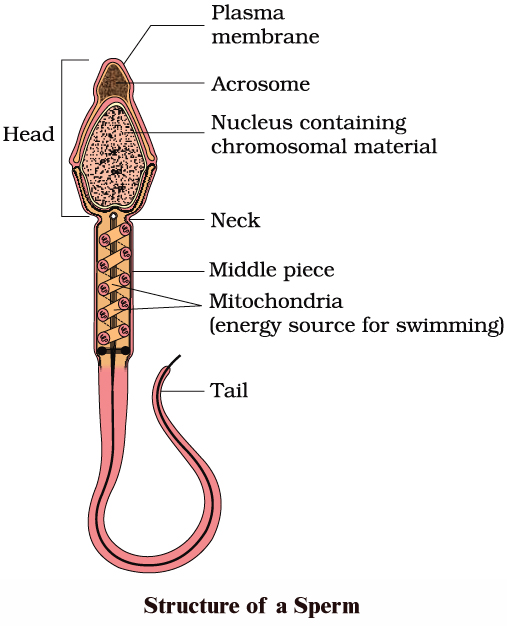
Transformation of spermatid to sperms is termed spermiogenesis. A spermatid is non-motile. It has organelles like mitochondria, Golgi bodies, centrioles, nucleus etc.
During spermiogenesis, the weight of gamete is reduced along with development of locomotory structures. Nucleus becomes compact forming the major part of head of spermatozoa,
Golgi complex of spermatid give rise to acrosome. Acrosome forms a cap in front of nucleus containing lytic agent which dissolves egg membranes during fertilization.
Acrosome of mammalian sperm produces sperm lysins. The two centrioles of the spermatids become arranged one after the other behind the nucleus. The anterior one is known as the proximal centriole.
The proximal centriole is usually located on the neck of spermatozoan. During fertilization, it is introduced in to the egg and is required for the first cleavage.
The posterior centriole is known as the distal centriole and gives rise to the axial filament of the sperm. Mitochondria from different parts of spermatid to get arranged in the middle piece around the axial filament.
Mitochondria in the middle piece provide energy to the sperm for locomotion.
A typical mammalian sperm is flagellated, consisting of four parts namely head, neck, middle piece and tail.
The human sperm was first seen by Hamm and Leeuwenhoek. Tail-less, (non-flagellate) 'amoeboid' sperm is found in the roundworm Ascaris.
Hormonal control of spermatogenesis
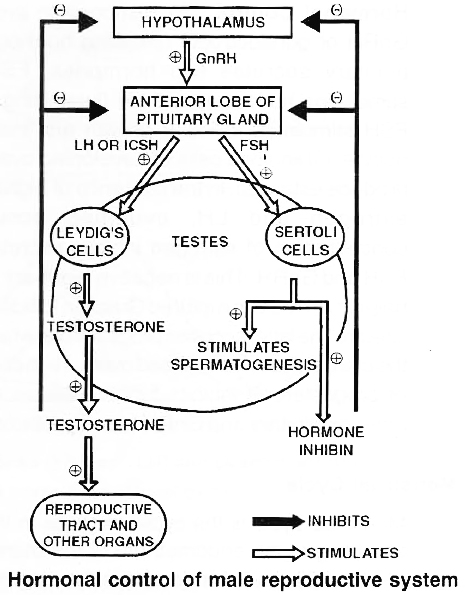
Spermatogenesis is under the control of endocrine hormones. Hypothalamus produces gonadotropin releasing hormone or GnRH.
It acts on anterior pituitary to produce gonadotropins, ICSH and FSH, ICSH interstitial cell stimulating hormone acts on interstitial or Leydig cells which produce testosterone.
Testosterone is essential for formation of sperms, atleast spermiogenesis part by Sertoli cells. Under the influence of FSH, Sertoli cells develop androgen binding protein (ASP).
The latter helps in concentrating testosterone in the seminiferous tubules.
Excess of testosterone inhibits LH/ICSH by anterior pituitary and GnRH production by hypothalamus.
Sertoli cells also produce a glycoprotein called inhibin. Inhibin suppresses FSH synthesis by anterior pituitary and GnRH synthesis by hypothalamus.
Thus normal release of testosterone is under negative feed back control.
OOGENESIS
Oogenesis is the process of maturation of reproductive cells in ovary. Oogenesis starts before birth. In 25 weeks old female foetus, all the oogonia are produced.
Oogenesis is basically similar to spermatogenesis. It includes phase of multiplication, phase of growth and phase of maturation.
During the phase of multiplication, the primordial cells in the ovary divide mitotically to form oogonia (egg mother cell). Each oogonium divides mitotically to form two primary oocytes.
Primary oocytes undergo growth, the growth phase during oogenesis is comparatively longer.
Primary oocytes, begin the first step of Meiosis-I and proceed up to diakinesis.
These oocytes resume their development at puberty. The primary oocyte (2n) completes meiosis-I producing two haploid cells (n), the larger one is secondary oocyte and the smaller one is first polar body.
Secondary oocyte starts Meiosis-II and proceeds upto metaphase-II only. Further development will start only after arrival of spermatozoa.
Entry of sperm restarts the cell cycle by breaking down M PF (M-phase promoting factor) and turning on APC (Anaphase promoting complex). Completion of meiosis II results in the formation of functional egg or ovum and a second polar body.
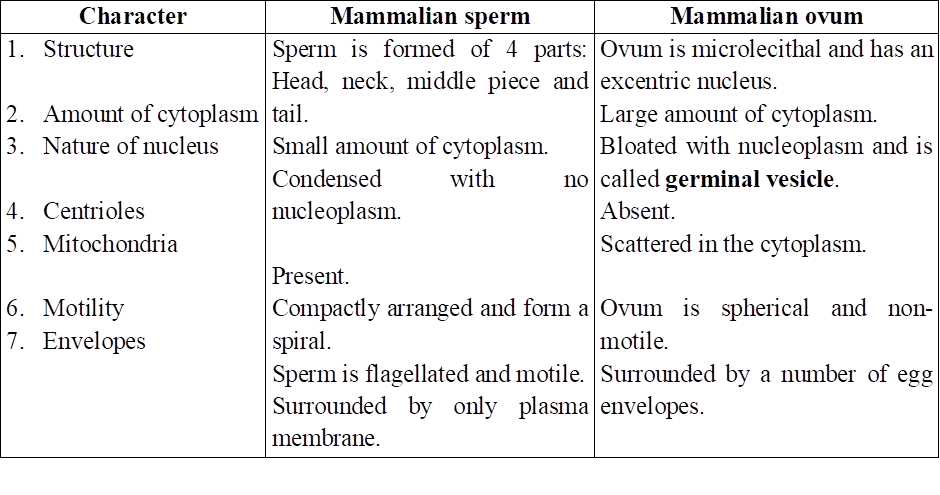
Compare the structure of Mammalian sperm and Mammalian ovum
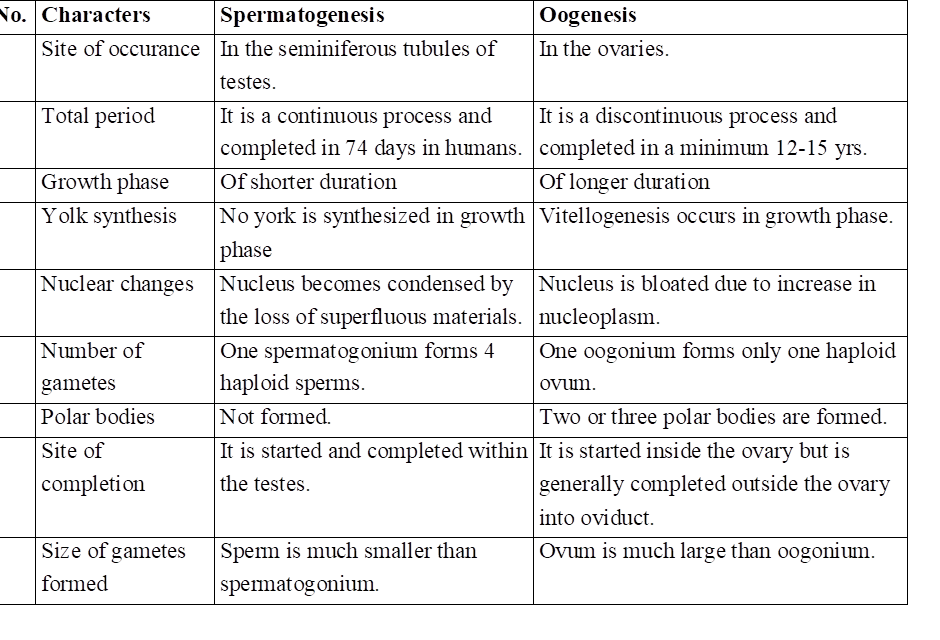
Differences between Spermatogenesis and Oogenesis
Hormonal control of Oogenesis
In response to production of GnRH or gonadotropin releasing hormone, anterior pituitary secretes two hormones, FSH (follicle stimulating hormone) and LH (luteinizing hormone).
FSH stimulates follicular growth and maturation of oocyte. Granulosa cells of developing ovarian follicle produce estrogen.
In presence of high titre of both estrogen and LH, ovulation occurs. High concentration of estrogen inhibits secretion of both FSH and GnRH.
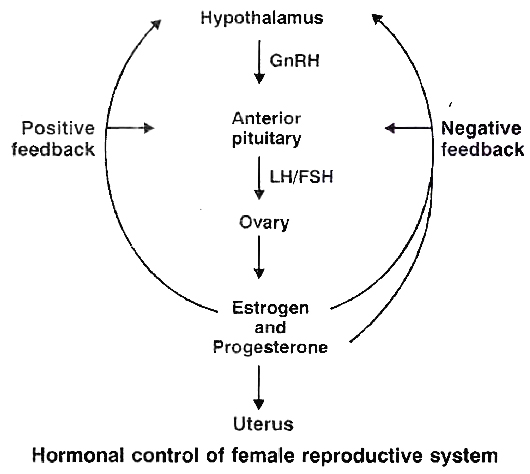
This is negative feedback control LH helps in converting ruptured Graafian follicle into corpus luteum.
The latter secretes progesterone which prepares the uterus to receive fertilised ovum. High concentration of progesterone inhibits further release of LH from anterior pituitary and GnRH from hypothalamus.
menstrual cycle
- Books Name
- A TEXT OF BIOLOGY - CLASS XII
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 12
- Subject
- Biology
MENSTRUAL CYCLE
Menstrual cycle is the cyclic changes in the reproductive tract of primate (Man, Monkey and Apes) females. Menstruation is the periodic shedding of the endometrium of uterus with bleeding. In healthy women, menstruation occurs at intervals of about 28 to 29 days.
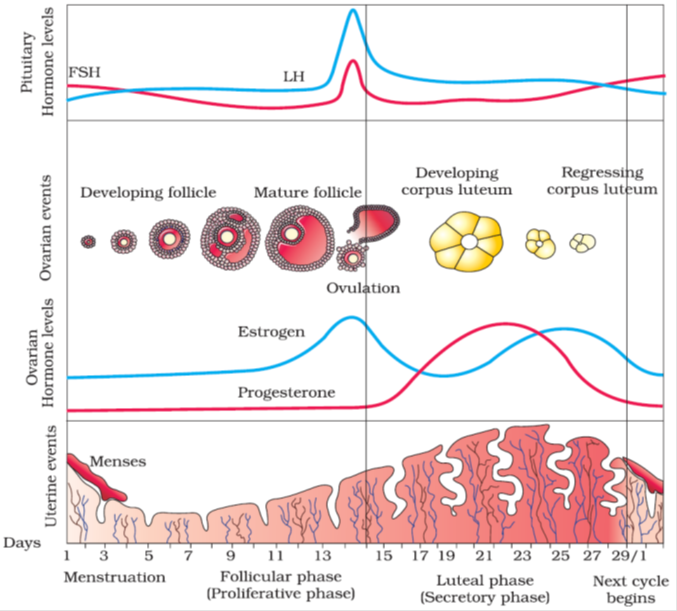
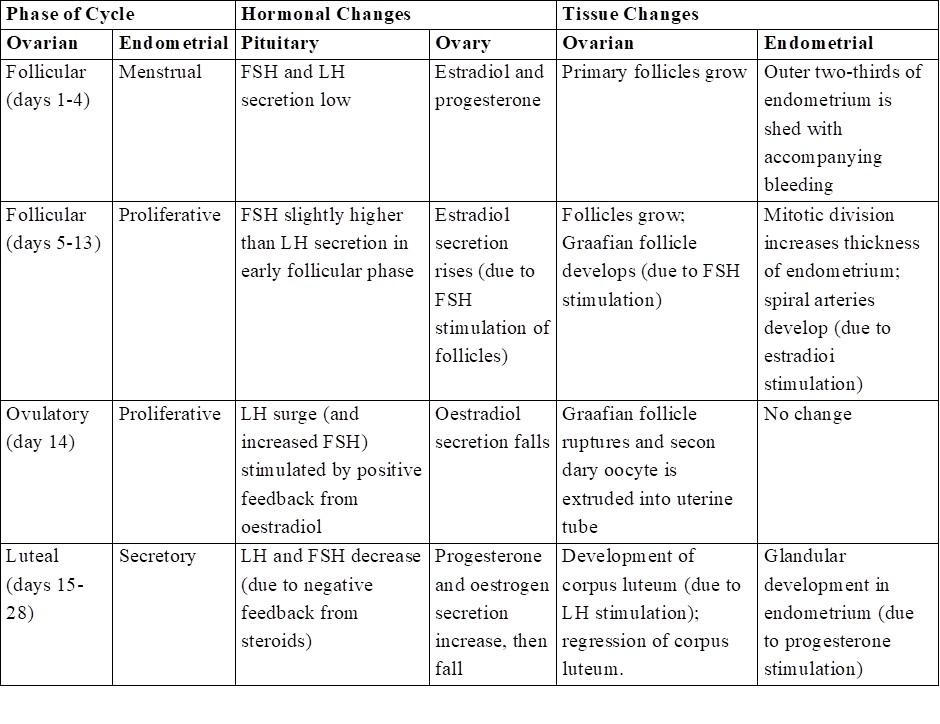
Menarche is the starting of menstruation in girls that occurs at about 13 years of her age. Menstrual cycle consists of menstrual phase, proliferative phase (follicular phase) and secretory phase (luteal phase).
Proliferative phase (5th to 14th day of menstrual cycle) consists of growth of endometrium of uterus, fallopian tube and vagina. In ovary, a Graafian follicle secretes estrogen during this phase.
Estrogen is the hormone active during proliferative phase. The ovum is released from the follicle near the end of proliferative phase, i.e., 14th day or midway during menstrual cycle.
Ovulation occurs under the influence of LH from pituitary. The subsequent 14 days in which corpus luteum is active is referred to as the secretory phase.
Progesterone secreted by corpus luteum is active during secretory phase. The uterine endometrium and glands grow further during secretory phase.
At the end of secretory phase, corpus luteum degenerates into corpus albicans in the ovary, progesterone secretion falls, the overgrown uterine endometrium breaks down and mensturation takes place.
Menstrual cycle is controlled by FSH, LH, estrogen and progesterone. The menstrual cycle and menstruation remain suspended during pregnancy and lactation. Menopause (climacteric) is the period of life when menstruation naturally stops.
Menopause occurs in females at the age of around 45-50 years. Ability to reproduce is lost in the female after menopause.
Various Phases of the Menstrual Cycle
ESTROUS CYCLE
The estrous cycle consists of cyclic changes in the female reproductive system of non-primate mammals. There is no menstruation at the end of estrous cycle.
The estrogen level in blood increases resulting strong sex urge in the female. This is called "period of heat".
The estrous cycles run only during breeding season. The estrous cycles remain suspended in female during non-breeding season. The suspension of estrous cycles is called the state of anestrum.
Those animals that have only a single estrous during the breeding season are called monoestrous, e.g., dog, fox, deer, bat, etc.
The animals that have a recurrence of estrous during breeding season are called polyestrous, e.g., Mouse, squirrel, cow, sheep, pig, horse etc.
Concept Builder
Types of Egg
The eggs are classified on the basis of amount and distribution of yolk in them. Yolk is the reserve food material in the cytoplasm of egg. It may be formed of phospholipids, proteins, or lipid and carbohydrates. The process of formation of yolk and its deposition in egg. is called vitellogenesis.
1. Based on amount of yolk.
(i) Alecithal -Eggs without yolk e.g. human egg.
(ii) Microlecithal -The eggs with very little yolk, e.g. sea urchin, starfish.
(iii) Mesolecithal -The eggs containing moderate amount of yolk, e.g. frog.
(iv) Megalecithal (or Macrolecithal) -The eggs containing very large amount of yolk, e.g. reptiles, birds.
2. Based on distribution of yolk.
On the basis of distribution of yolk, the eggs are classified as follows
(i) Isolecithal -The yolk is uniformly distributed throughout the cytoplasm of egg, e.g., Branchiostoma, Herdmania.
(ii) Telolecithal-The eggs in which the yolk is concentrated towards one pole i.e., vegetal pole & nucleus along with major part of cytoplasm is displaced is animal pole e.g. , amphibians.
(iii) Centrolecithal -Yolk concentrated in centre of the egg with cytoplasm surrounding it, e.g. insects.
Cleidoic Eggs
Eggs of reptiles and birds are insulated by albumen, membranes and shell. The calcareous shell present around the eggs of bird is mainly made up of calcium carbonate (94%) and is secreted by uterus (shell glands). Chalazae are the suspensory ligaments of the yolk in birds's egg.
Egg Membranes
There are three types of egg membrane which can be present around the egg
(i) Primary egg membrane: It is formed around the plasma membrane of egg secreted by ovum itself e.g, Jelly envelope (Echinoderms). Vitelline membrane (Mollusca, amphibians & birds), zona radiata (Shark, some amphibians).
(ii) Secondary egg membrane: It is formed around an egg by the follicle cells of the ovary e.g., chorion around egg of insect; corona radiata, granulosa & theca layers in human.
(iii) Tertiary egg membranes: These are formed by the oviducts & other accessory parts of maternal genital tract while the egg is passing from the ovary to the exterior. e.g., the albumin, shell membrane & outermost calcareous shell of reptiles & birds.
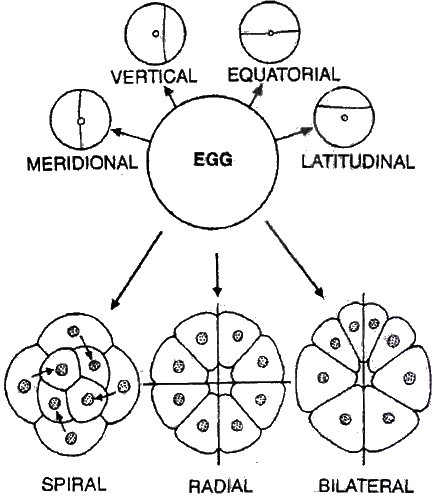
Types of Cleavage
The mode of cleavage is determined by the amount of yolk and its distribution.
(a) Holoblastic: The cleavage in which the segmentation lines pass through the entire egg , dividing it completely. It occurs in alecithal, microlecithal and mesolecithal eggs; e.g. frog, human egg etc. It is of two types equal holoblastic example Amphioxus and Marsupials; unequal holoblastic e.g., lower fishes and amphibians.
(b) Meroblastic: The lines of segmentation do not completely pass through the egg and remain confined to a part of the egg. Such type of cleavage is found in megalecithal eggs as the yolk provides resistance to the cleavage, e.g. insects, birds, reptiles. Meroblastic cleavage may be (i) Superficial which occurs in centrolecithal eggs, e.g . insects, or (ii) discoidal, found in eggs of birds.
Patterns of Cleavage
Cleavage is the successive mitotic cell divisions of the egg & can be in following pattern
(i) Radial Cleavage: Successive clevage plane cuts straight through the egg e.g. Synapta paracen rotus.
(ii) Biradial Cleavage: When the first three division planes do not stand at right angles to each other: Ctenophora
(iii) Spiral Cleavage: There is a rotational movement of cell parts around the egg axis leading to displacement of mitotic spindle with respect to symmetrically disposed radii e.g. turbellarians, nematoda, rotifera, annelida, all mollusc except cephalopods.
(iv) Bilateral Cleavage: Mitotic spindles and cleavage planes remain bilaterally arranged with reference to the plane of symmetery e.g. tunicates, Amphioxous, amphibia and higher mammals.
(v) Meridional Cleavage: When cleavage furrow bisects both the poles of egg passing through animal vegetal axis, the plane of cleavage is called meridional cleavage.
According to the concept of potency, cleavage can be
(i) Indeterminate/Regulative eggs, the fate of different parts of egg or its blastomeres is not predetermined or blastomeres have no characterstic position & alterable fate e.g. Echinoderms and vertebrates.
(ii) Determinate/Mosaic eggs. Every part of fertilized egg has a definite fate, so that fate of every blastomere is determined from beginning i.e. , produces the complete embryo only if all the blastomeres remain together. e.g., Nematoda, Mollusca (Dentalium).
Morula
Cleavage results in the formation of solid mass of cells called Morula as it looks like a mulberry.
Blastula
Blastula is the embryonic stage next to morula.
It contains a fluid-filled cavity called blastocoel surrounded by one or more layers of cells, the blastomeres.
The blastula with blastocoel is called coeloblastula, e.g. frog.
In certain animals, the blastula is solid and is termed stereoblastula e.g., Cnidaria, Nereis & some molluscs.
The blastula formed as a result of superficial cleavage is called superficial blastula, e.g. insects.
Discoblastula is disc shaped blastula formed as a result of discoidal cleavage, e.g. birds.
Gastrula
Gastrula is formed by gastrulation. Gastrulation is the process of the formation of gastrula from the blastula. Gastrula is the embryonic stage of development in which the germinal layers are formed. Gastrulation involves movement of cells.
The movements are called morphogenic movements. They include epiboly (descending of dividing cells to cover other cells) , emboly (upward movement of dividing cells underneath the other cells), involution (inward migration of blastomeres to go into the blastocoel), invagination (tucking in of blastula wall) , and delamination (separation of a sheet of cells from blastula) .
Archenteron is the cavity which occurs inside the gastrula, and is the future alimentary canal. It opens to the outside through blastopore which closes later.
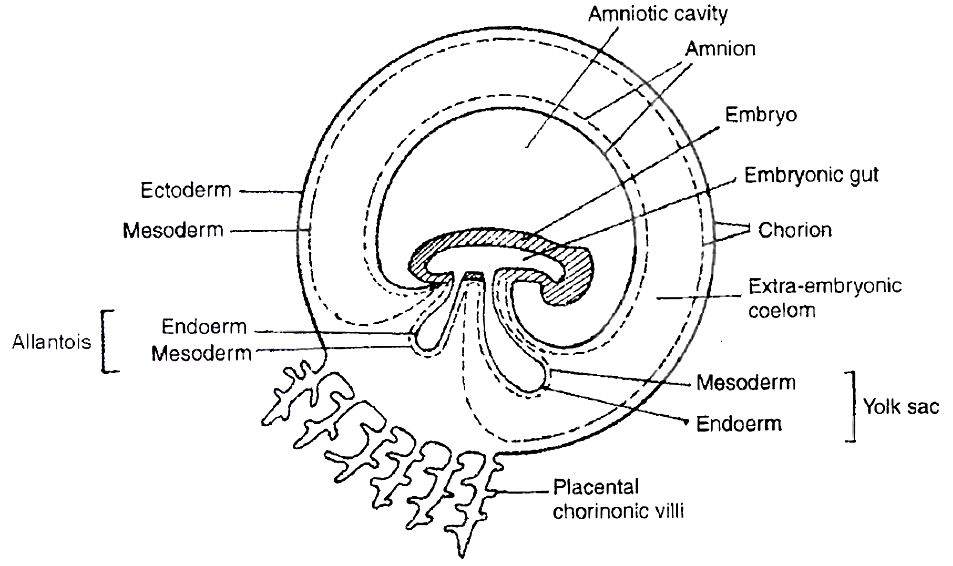
Foetal Membranes (Extra embryonic membranes)
The developing foetus is enclosed by three membranes, amnion, chorion and allantois.
(i) Amnion is formed from mesoderm outside and ectoderm inside. Space between amnion and foetus is called amniotic cavity and it contains amniotic fluid.
(ii) Chorion is formed from ectoderm externally and mesoderm inside. Alongwith the allantois it participates in the formation of placenta. Space between amnion and chorion is embryonic coelom .
(iii) Allantois consists of mesoderm outside, and endoderm inside. It extends to fuse with chorion and forms allanto-chorion which gives rise to foetal part of placenta.
fertilisation and implantation
- Books Name
- A TEXT OF BIOLOGY - CLASS XII
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 12
- Subject
- Biology
THE EVENTS IN MAMMALIAN REPRODUCTION
FERTILISATION
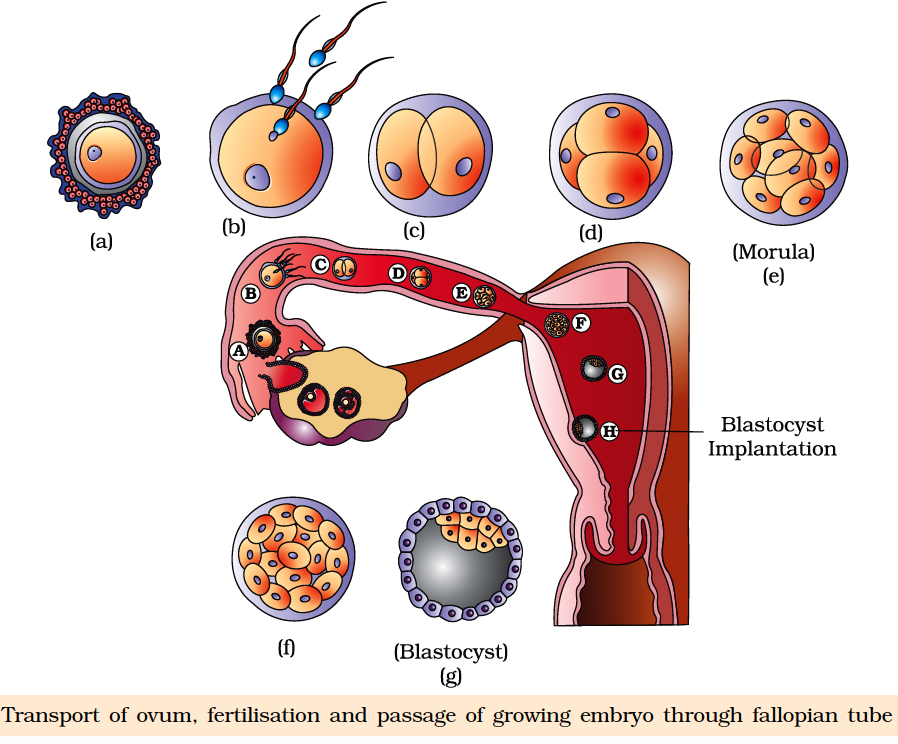
Ovum is released in the secondary oocyte stage (arrested in metaphase-II). Due to ciliary current produced by fimbriae of oviduct, ovum is drawn in through ostium.
It reaches ampulla, the site of fertilisation, by the ciliary action of ciliated columnar epithelium lining of oviduct.
A human sperm can live for many weeks in male genitial duct. Once ejaculated sperm can live alive only for 24 to 48 hours outside the body. Sperms move in the liquid medium secreted by female genital tract (1.5-3.0 mm/minute).
Prostaglandins of semen help in movement of spermatozoa and finally reach ampulla portion of the oviduct.
Capacitation of sperm occurs in the female genital system due to
(1) Removal of membrane cholesterol present over acrosome, weakening the membrane cover.
(2) Dilution of decapacitation factors.
(3) Entry of Ca2+ into sperms causing rapid whiplash motion of the tail.
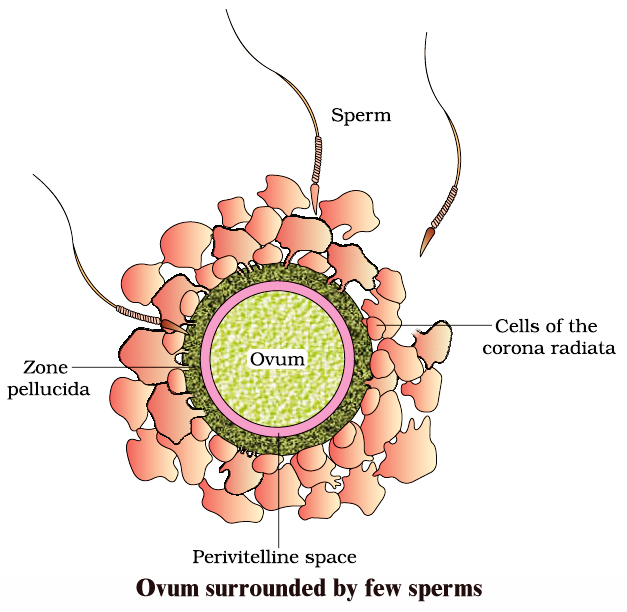
Fusion of gametes/Syngamy: The various steps involve :
Acrosomal reaction: Number of sperms adhare to the surface of egg covers (Agglutination). The acrosome starts releasing its hydrolytic enzymes (sperm lysins).
It includes,
(a) Hyaluronidase: Dissolves the hyaluronic acid responsible for cementing of follicle cells or granulosa cells.
(b) Corona digesting enzyme (CDE) : Dissolves corona radiata.
(c) Zona lysin/Acrosin : Digests the zona pellucida. It involves zona pellucida compatibility reaction determined by 'fertilizin' protein over zona pellucida and 'antifertilizin' in case of sperm.
Contact of acrosome stimulates development of an outgrowth by the oocyte called fertilisation cone or cone of reception.
As the sperm head gets in contact with the fertilization cone, it cause opening up of Na+ channel to cause depolarisation of membrane (fast block to check polyspermy) and Ca2+ wave inside the egg.
Sperm and egg membranes dissolve. Male pronucleus & proximal centriole of sperm enter the cytoplasm of egg & rest part is left out.
Ca2+ wave causes extrusion of cortical granules (cortical reaction) and zona reaction makes the zona pellucida impervious to second sperm by destroying sperm receptors.
Cortical reaction and zona reaction constitute slow block to check polyspermy.
Entry of sperm causing breakdown of metaphase promoting factor (MPF) and turning on anaphase promoting complex (APC). This results in oocyte completing its meiosis -II.
Male and female pronuclei approach each other and finally mixing up of paternal and maternal chromosomes (Amphimixis) occur resulting in the formation of zygote/ synkaryon.
embryonic development
- Books Name
- A TEXT OF BIOLOGY - CLASS XII
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 12
- Subject
- Biology
EMBRYONIC DEVELOPMENT
It includes cleavage, blastulation, implantation, gastrulation and organogenesis.
Cleavage:
First cleavage is completed after 30 hours of fertilization. Cleavage furrow passes from animal-vegetal axis as well as centre of zygote (Meridional cleavage).
It divides the zygote into two blastomeres (Holoblastic cleavage). Second cleavage is completed after 60 hours of fertilization.
It is also meridional but at right angle to the first one. It is completed earlier in one of the two blastomeres resulting in transient 3-celled stage.
Third cleavage is horizontal forming 8 blastomeres. lt is slightly unequal. Thereafterthe rate and pattern of cleavage is not specific.
Morula:
Cleavage results in solid ball of celled Morula with 16 cells (occasionally 32 cells). Zona pellucida is still present as the outer cover. Morula undergoes compaction.
The outer/peripheral cells are small/flat with tight junction while the inner cell mass slightly large round and with gap junction.
Morula descends slowly towards uterus in 4-6 days and corona radiata detaches during this period.
BLASTULATION OR BLASTOCYST FORMATION
Endometrium secretes a nutrient fluid and its mucosal cells become enlarged with stored nutrients. As the morula enters uterus, it obtains enriched supply of nutrients.
Outer peripheral cells enlarge and flatten further. They form trophoblast or trophoectoderm. Trophoblast secretes a fluid into the interior. It creates a cavity called blastocoel.
The inner cell mass now comes to lie on one side as embryonal knob.
With the formation of blastocoel, morula is converted into blastula which is called blastocyst in mammals because of different nature of surface layer and eccentric inner cell mass.
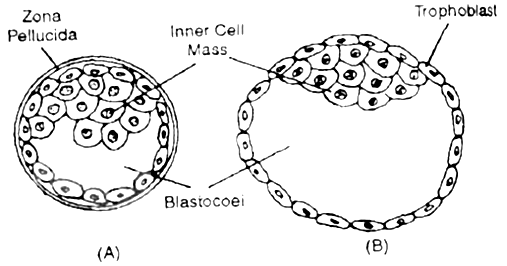
Due to pressure of growing blastocyst a slit is produced in zona pellucida. The growing blastocyst comes out. At times it gets broken into two parts which then give rise to identical twins.
Trophoblast cells in contact with embryonal knob are called cells of Rauber. Area of embryonal knob represents animal pole.
The opposite side is embryonal pole. Soon embryonal knob shows rearrangement to form embryonal disc. Cells of trophoblast layer divide periclinally.
This makes trophoblast two layered, outer syncytotrophoblast and inner cytotrophoblast. The two layers later form chorion, amnion and foetal part of placenta.
IMPLANTATION
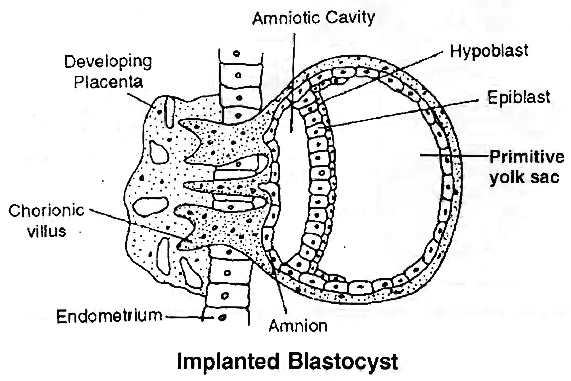
It is embedding of the blastocyst into endometrium of uterus.
Blastocyst comes in contact with the endometrium in the region of embryonal knob or embryonic disc. It adheres to the same.
The surface cells of trophoblast secrete lytic enzymes which cause corrosion of endometrial lining.
They also give rise to finger-like outgrowths called villi. Villi not only help in fixation but also absorption of nourishment.
Implantation causes nutrient enrichment, enlargement of cells and formation of uterine part of placenta called decidua (L. deciduus-falling off).
Decidua has three regions (i) Decidua Basalis (Basal Decidua, Tunica Serotina). Part of decidua underlying the chorionic villi and overlying the myometrium. (ii) Decidua Capsularis (Decidua Reflexa). It lies between embryo and lumen of uterus. (iii) Decidua Parietalis (Decidua Vera).
It is part of decidua that lines the uterus at a place other than the site of attachment of embryo.
Trophoblast secretes hormone called human chorionic gonadotropin (hCG). Detection of hCG in the urine is the basis of pregnancy/Gravidex test.
hCG maintains the corpus luteum beyond its normal life. It continues to secrete progesterone which prevents menstruation and maintains the uterine lining in nutrient rich state.
Progesterone induces the cervical glands to secrete viscous mucus for filling the cervical canal to form a protective plug.
Progesterone is also called pregnancy hormone as it is essential for maintenance of pregnancy. The hormone is secreted by placenta as well.
GASTRULATION
It is characterised by movement of cells in small masses or sheets so as to form primary germinal layers. There are three primary germinal layers -endoderm, ectoderm and mesoderm.
The cell movements that occur during gastrulation are called morphogenetic movements since they lead to initiation of morphogenesis. The product of gastrulation is called gastrula.
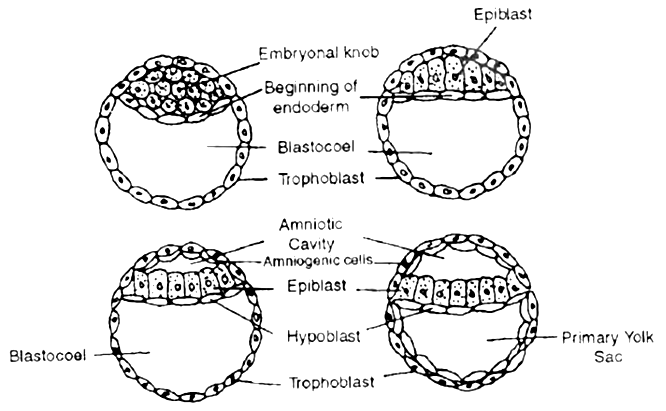
 Formation of endoderm, and amniotic cavity
Formation of endoderm, and amniotic cavityFORMATION OF PRIMARY GERMINAL LAYERS
Cells of the inner cell mass or embryonal knob get rearranged to form a flat embryonic or germinal disc. The latter differentiate into two layers, outer epiblast of larger columnar cells and inner hypoblast of smaller cuboidal cells.
Gastrulation begins with the formation of the primitive streak on the surface of the epiblast.
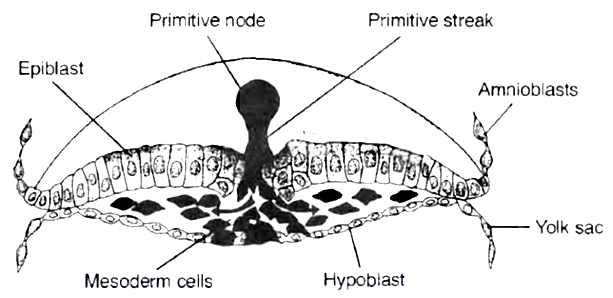
 1. Cross section through the cranial, region of the streak at 15 days showing movement of epiblast cells. The first cells to move inward displace the hypoblast to create the definitive endoderm.
1. Cross section through the cranial, region of the streak at 15 days showing movement of epiblast cells. The first cells to move inward displace the hypoblast to create the definitive endoderm.
2. Once definitive endoderm is established, inwardly moving epiblast forms mesoderm.
3. Cells remaining in the epiblast form ectoderm. Thus the epiblast is the source of all the germ layers in the embryo.
FATE OF GERM LAYERS
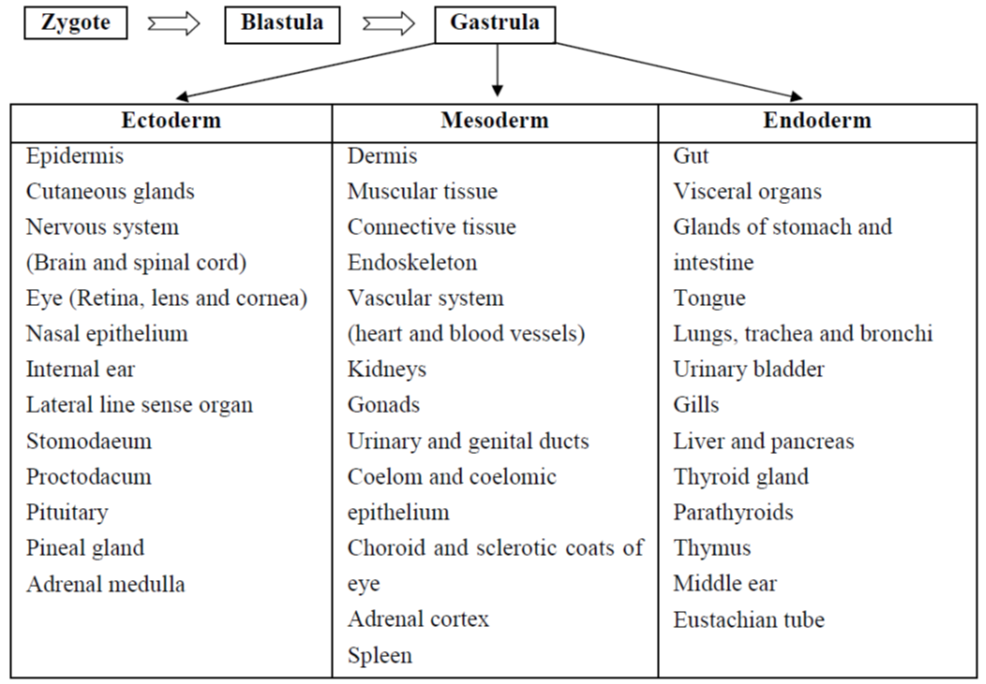
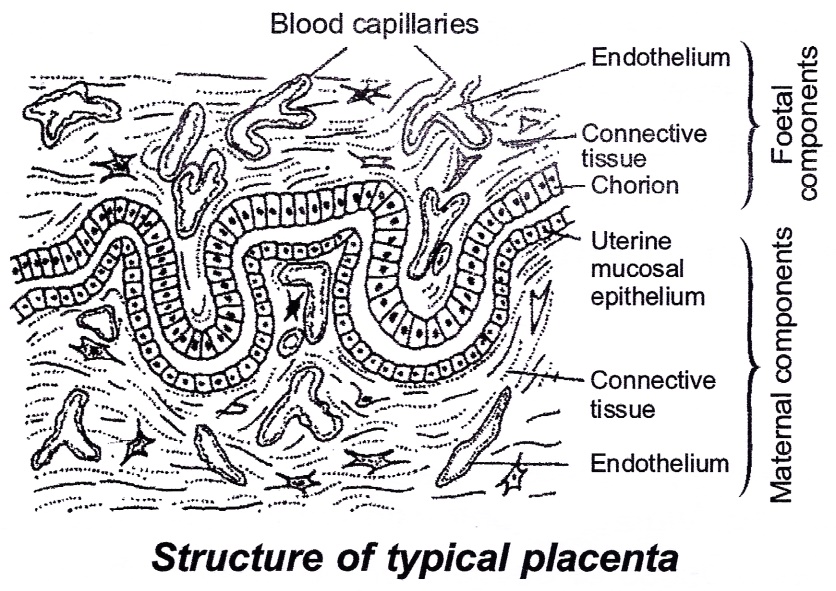
PLACENTA
Placenta is an organ which connects the foetus and uterine wall.
It is contributed by both-maternal as well as foetal part although there is no blending of the maternal and foetal blood supplies, the placenta acts as an ultrafilter, soluble inorganic and organic materials nutrients, hormones, antibodies against diphtheria, small pox, scarlet fever, measles, etc. can pass from the mother to the foetus.
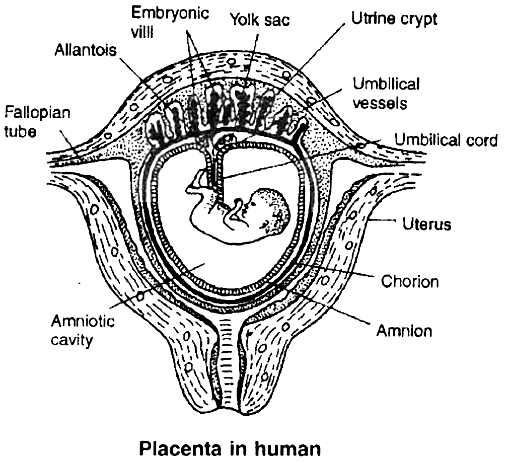
Placenta acts as an endocrine gland and synthesises large quantities of proteins and some hormones, such as human chorionic gonadotropin (hCG), chorionic thyrotropin, chorionic corticotropin, chorionic somatomammotropin, estrogens and progesterone.
The hCG stimulates the corpus luteum to secrete progesterone until the end of pregnancy. In addition, it secretes relaxin that facilitates parturition by softening the connective tissue of the symphysis pubica.
The metabolic activity of the placenta is almost as great as that of the foetus itself. The umbilical cord connects the foetus to the placenta.
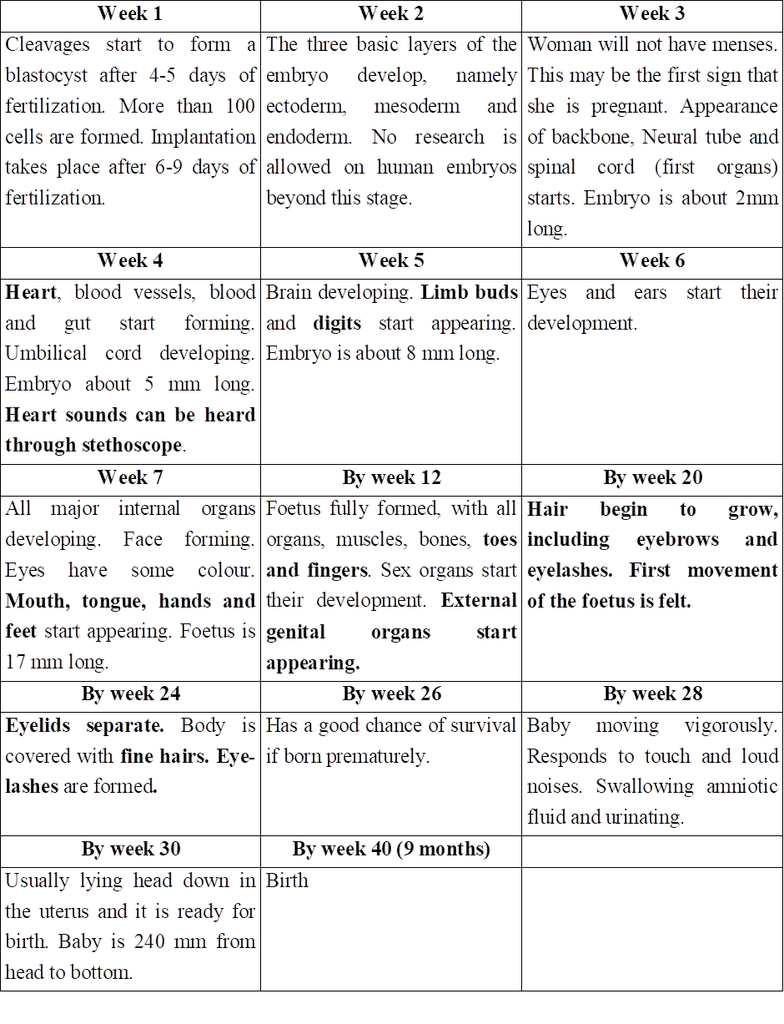
During the first trimester (first 3 months) of pregnancy, the basic structure of the baby is formed.
This involves cell division, cell migration, and the differentiation of cells into many types found in the baby. During this period, the developing baby-called foetus is very sensitive to anything that interferes with the steps involved.
Virus infection of the mother e.g., by Rubella (German measles) virus or exposure to certain chemicals, may cause malformations in the developing embryo. Such agents are called teratogens (monster forming).
By 3 months, all the systems of the baby have been formed, at least in a rudimentary form.
From then, development of the foetus is primarily a matter of growth and minor structural modifications.
The foetus is less susceptible to teratogens.
Table-I: Important Developmental Events in the Human Embryo
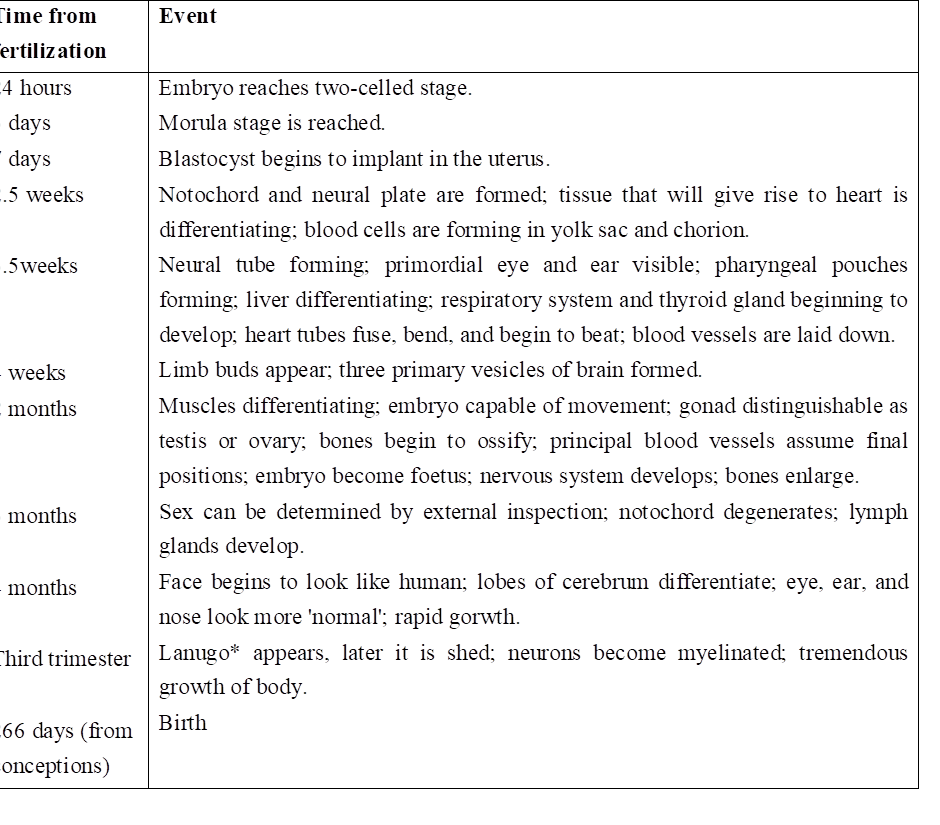
* Lanugo is the soft hairy covering of the foetus which begins to be shed before birth.
parturition and lactation
- Books Name
- A TEXT OF BIOLOGY - CLASS XII
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 12
- Subject
- Biology
PARTURITION
The gestation period of the human is about 38 weeks/266 days followed by birth. The process of giving birth to a baby is called parturition.
It starts with rise in estrogen/progesterone ratio, increase in the level of oxytocin secretion by both, mother and foetus.
It includes 3 stages.
1. Dilation Stage:
The uterine contraction starts from top and occur at long intervals (once every thirty minutes). This forces the baby to push its head against cervix.
As a result, cervix gets dilated with vagina also showing similar dilation. Dilation of cervix increases the stimulus for oxytocin secretion, further increasing the strength and frequency of contractions (1-3 every minute).
With continued powerful contractions, the amnion ruptures and the amniotic fluid flows out through vagina.
2. Expulsion Stage:
With further increase in the intensity of uterine and abdominal contraction, the baby comes out through cervix and vagina with head coming out first.
It may take 20 -60 min. Umbilical cord is cut. The infant's lungs expand and it begins breathing. This requires a major switch over in the circulatory system.
Blood flow through the umbilical cord ductus arteriosus and foramen ovale ceases; the adult pattern of blood flow through the heart, aorta and pulmonary arteries begins.
In some infants, the switch over is incomplete, and blood flow through the pulmonary arteries is inadequate. Failure to synthesise enough nitric oxide (NO) is one cause.
3. After Birth:
Within 10-15 minutes after delivery, the placenta and the remains of the umbilical cord which is called 'after birth' is expelled out.
LACTATION
Although estrogen and progesterone are essential for the physical development of the breasts during pregnancy, a specific effect of both these hormones is to inhibit the actual secretion of milk. Conversely, the hormone prolactin has exactly the opposite effect on secretion: promotion of milk secretion.
This hormone is secreted by the mother's anterior pituitary gland and its concentration in her blood rises steadily from the fifth week of pregnancy until birth of the baby, at that time it has risen to 10 to 20 times the normal nonpregnant level.
In addition, the placenta secretes large quantities of human chorionic somatomammotropin, which probably also has lactogenic' properties, thus supporting the prolactin from the mother's pituitary during pregnancy.
The fluid that is secreted in the last few days before and first few days after parturition is called colostrum, it contains essentially the same concentrations of proteins and lactose as milk but almost no fat.
Ejection (or "Let-Down") Process in Milk Secretion
Milk is secreted continuously into the alveoli of the breasts, but milk does not flow easily from the alveoli into the duct system and, therefore, does not continually leak from the breast nipples.
Instead, the milk must be ejected from the alveoli into the ducts before the baby can obtain it. This is caused by a combined neurogenic and hormonal reflex that involves the posterior pituitary hormone oxytocin.
When the baby suckles, sensory impulses are transmitted through somatic nerves from the nipples to the mother's spinal cord and then to her hypothalamus, there causing nerve signals that promote oxytocin secretion at the same time they cause prolactin secretion.
The oxytocin is carried in the blood to the breasts, where it causes myoepithelial cells (that surround the outer walls of the alveoli) to contract, thereby expelling the milk from the alveoli into the ducts.
Summary of Human Pregnancy from Fertilization to Birth of the Baby
Concept Builder
Types of Placenta
(a) On the basis of structure, the placentae are of following types:
(i) Epitheliochorial - Placenta with all the six barriers between foetal and maternal blood; e.g. Horse, Ass.
(ii) Syndesmochorial - Uterine epithelium breaks down; only five barriers left; e.g. Cow, Buffalo, Sheep, Goat, Camel.
(iii) Endotheliochorial - Uterine epithelium and connective tissue eroded; only four barriers left; e.g. Tiger, Lion, Cat, Dog.
(iv) Haemochorial - Placenta with only three barriers, the maternal part of placenta eroded; e.g. Human, Ape, Lemurs.
(v) Haemo-endothelial-All barriers except endothelium of foetal part of placenta get eroded e.g. Rat, Rabbit.
(b) On the basis of nature of uterine wall after parturition, the placenta may be :
(i) Non-deciduous-no part of uterine portion of placenta is broken off, e.g. Horse, Ass.
(ii) Deciduous-a portion of uterine tissue called decidua is detached and passed out at birth, e.g. most of the mammals.
(iii) Contra deciduous – even the foetal part of placenta is retained and gets absorbed to provide nourishment, e.g. Talpa, Parameles.
(c) On the basis of distribution of villi on the surface, the placentas are categorised into six types :
(i) Diffuse placenta-Villi distributed uniformly all over the surface. e.g. Horse, Pig .
(ii) Cotyledonary-the villi form tufts which fit into corresponding areas, the caruncles in uterine part of placenta, e.g.' Cow, Buffalo, Sheep.
(iii) Intermediate-villi occur singly as well as in tufts, e.g. Camel, Giraffe
(iv) Zonary-villi arranged in two transverse bands, e.g. Tiger, Lion, Cat, Dog, Elephant.
(v) Discoidal-When the villi are confined to a disc-like area, e.g. Rat, Rabbit, Bat.
(vi) Metadiscoidal-The placenta in which the villi are initially distributed uniformly all over the surface but later on get confined to a disc-like area fitting into a corresponding depression on the uterine wall. That is, the placenta is diffuse at first but later on becomes discoidal, e.g. Human beings and Apes.
Concept Builder
1. Amenorrhoea: Non occurrence of menses.
2. Inguinal hernia: Protrusion of intestinal loop into scrotum
3. Spontaneous ovulator : Ovulation with any external induction.
4. Orchidectomy: Removal of testes. It produces eunuchs.
5. Induced ovulator : Ovulation after copulation e.g., Rabbit.
6. Hysterectomy: Surgical removal of uterus.
7. Unejaculated sperms: Sperm production is a continuous process. unejaculated sperms are absorbed in vas deferens.
8. Corpus luteum : Persists for two weeks in case of non-pregnancy and four months when pregnancy has taken place.
9. Cryptorchidism: Failure of testes to descend in to scrotum.
10. Spermatogenesis takes about 74 days.
11. Androgenesis: Development in which the embryo has only paternal chromosomes, male parthenogenesis.
12. Gynogenesis : Development in which the embryo has only female chromosomes, female parthenogenesis.
13. Mictic females produce: haploid eggs which can be fertilized by males. Amictic females produce diploid eggs which develop parthenogenetically. A diploid egg may be produced by -autofertilization (polar body fuses with secondary oocyte) or Restitution: Chromosomes of both secondary oocyte and polar bodies arrange at equator during 1st cleavage e.g. hymenopterans (bees and wasps)
14. Paras: Fertile, can have pregnancy
15. Nulliparous: Women with no children
16. The most common method by which a baby comes out at parturition is left anterior oblique with head coming out first.
17. Fetal hemoglobin differs from adult hemoglobin because it has and chains. It has higher affinity for O2 and shifts HbO2 dissociation curve to left.
18. 1st Menses is called menarche while the onset of menses and development of secondary sexual characters is called puberty. Dysmenorrhoea - painful menses.
19. In the three trimesters of preganancy. (0-12 weeks 12-22 weeks and 22-28 weeks) if the baby dies from 0-22 weeks by natural or man-made causes it is called abortion because embryo is not called viable.
20. After 20-22 weeks abortion is banned in India.
21. The number of eggs at the time of birth in a young female undergoes drastic reduction by a process called atresia.
22. Gynandromorphs: An individual possessing both male and female parts.
23. Menopause: Stopping of menses, average age 51 years. Post menopausal effects includes increased risk to heart attack due to decreased estrogens, hot flushes, irritability, fatigue, anxiety decreased strength of bones.
24. Implantation takes place in 7 days. Conceptus remains in fallopian tube for 3-4 days and then by 7-9 days implantation occurs.
25. Vasectomy : Cutting of vas deferens.
26. Gynaecomastia: Males developing breasts due to hormonal imbalances.
Gestation: The period of development of the young in the womb of the mother is called gestation. Maximum weight gain and maximum growth rate of foetus takes place between 7-9 months of pregnancy.
27. Human Egg 0.1 mm in diameter or 100 µm.
28. Human sperm 0.06 mm or 60 µm long
29. Largest sperm 5.8 cm (20 times longer than the body of fly) in Drosophila bifurca.
30. Ectopic Pregnancy : It is the growth of the foetus outside the uterus, commonly inside the fallopian tube. Hence also called as tubal pregnancy. By 6th week as growing foetus may cause rupturing of fallopian tube hence its immediate surgical removal.
31. Animal cloning: First performed by Willmut and Campbell (1997). The first cloned animal was sheep Dolly (Feb. 13, 1997). Egg cell was taken out when maturation promoting factors (MPF) were maximum. It was denucleated. A nucleus from udder cell arrested in non-dividing growth phase (GP) by serum starvation was inserted in the denucleated egg.
32. Spermatozoa of turbellarians and Ascaris (nematode) and sporozoans lack acrosome.
33. Non flagellate sperms are found in Ascaris, Procambarus (Crayfish) Callinectes (blue crab).
34. Biflagellate spermatozoa are found in Opsanus (toad fish)
35. Ascaris megalocephola univalens shows the process of chromosome dimunition. In these spiral clevage of egg takes place and each cell except the one giving rise to gametes looses a part of chromosome set. Other e.g. -Gall midges (Mayetiola) and fungus grats (Wachtiella)
36. Compact ovaries are found in -cyclostomes, elasmobranchs, osteichthyes fishes, reptiles, birds and mammals.
37. Saccular ovaries are found in amphibians.
38. Lampbrush chromosomes : Found in oocytes of amphibians. They resemble the brushes used to clean the chimneys in London. They store extra information for survival of egg. They consist of two homologous chromosomes held together at chiasmata present in (diplotene) prophase cell stage
39. Polytene chromosomes : Found in the interphase stage of cells of salivary glands of chromosomes of Drosophila larvae. They exhibit gene amplification.
40. Fecundity: Animals potential capability to produce off springs.
41. Fertility -Animal's actual capability to conceive or induce conception.
42. Precocial young ones: ungulates and jackrabits -hair and open eyes, ability to move around.
43. Altricial: young ones are naked blind and helpless.
44. Estrous cycle: When females are most receptive to male (not in man) -phases -Estrus -Metaestrus -Diestrus -Proestrus. It occurs in non-primates.
45. Rut cycle: Testicular activity in the majority of mammals, is a seasonal event as is the associated period of sexual excitement.
46. F.R. Lillie gave the fertilization theory. Fertilizin of egg of one species locks with antifertilizin of same species (1914).
47. Sperms are decapacitated in epididymis where they mature. They are recapacitated in vaginal fluid / uterus.
48. Spermetogensis : Is the process of formation of haploid sperm from the diploid primary spermatocyte in the testis.
49. Spermiogenesis : Is the process of transformation of haploid spermatid to the functional sperm.
50. Spermiation : Is the process of releasing the mature sperms from the semniferons tubuels.
51. Insemination : Is the process of introduction of sperms (or semen) in the female reproductive system.
52. Semination : Is the process of ejaculation of semen from the male reproductive system.
53. Menarche : Is the process of start of menstrual cycle in the life of a female human at puberty.
54. Follicular phase : Primary follicles in the ovary grow to become mature follicle (Graafian follicle).
55. Luteal phase : The process of transformation of ruptured Graafian follicle into corpus luteum.
56. Capacitation : Is the process of activation of sperms in the female reproductive system after their ejaculation into it.
 ACME SMART PUBLICATION
ACME SMART PUBLICATION
