- Books Name
- A TEXT OF BIOLOGY - CLASS XII
- Publication
- ACME SMART PUBLICATION
- Course
- CBSE Class 12
- Subject
- Biology
POPULATION EXPLOSION AND BIRTH CONTROL
Rapid increase in population over relatively short period is called population explosion.
Census gives information about the number of individuals present in a given region at a given time.
World Population 1900 2 billion
2000 6 billion
Indian Population 1947 350 million
2000 1 billion
It means every sixth person in the world is an Indian.
The time required for a population to double itself is called the doubling time.
The present growth rate of approximately 1.6 percent per year for India is smaller than the peak of about 2.1 percent per year during 1965-1970.
Population growth rate is indicated by (i) the annual average growth rate and (ii) the doubling time.
Growth rate depends on birth (fertility) rate, death (mortality) rate migration and age sex ratio.
The major reasons for this growth are :
(i) A rapid decline in death rate
(ii) A decline in maternal mortality rate (MMR)
(iii) A decline in infant mortality rate (IMR)
(iv) Increase in the number of people reaching reproducible age
BIRTH CONTROL
Is the process to prevent conception or pregnancy without interfering the reproductive health of the individuals.
Characteristics of an ideal contraceptive are: (i) User friendly, i.e., comfortable and easy to use. (ii) Without side effects. (iii) Reversible. (iv) Completely effective against pregnancy.
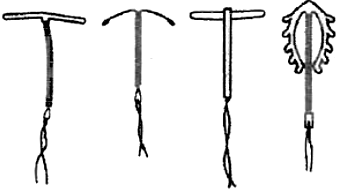
There are several methods of contraception-natural or traditional, barriers, IUDs, oral contraceptives, injectables, implants and surgical methods.
Couple protection is the process of bringing eligible couples under family planning measures. In India, it is over 55% at present and is voluntary in nature.
In 2004, there were 60·79 lakh IUD insertions, 48·74 lakh sterilisations, 249·9 lakh condom users and 87·54 lakh oral pill users.
METHODS OF BIRTH CONTROL
1. Natural Methods:
These are the methods which do not require any device or medicine so no side effects but chances of failure are very high.
Natural methods are of three kinds-safe period, withdrawal and breast feeding.
(i) Safe period (Rhythm Method) :
Ovulation occurs roughly about the middle of menstrual cycle.
Fertility period is upto 48 hours after ovulation, when fertilization can occur.
Avoiding sex during the fertility period will naturally prevent conception.
Ovulation period can be known by the rise in body temperature by about 1º F, cervical mucus is slippery and can be drawn into a thread (Spinnbarkeit test) when stretched between two fingers.
Period prior to ovulation is safe.
Period after fourth day of rise in body temperature (or last positive Spinnbarkeit test) is also considered safe.
It is however, always better to avoid sex from day 10-17 of the menstrual cycle.
(ii) Withdrawal Method (Coitus Intruptus) :
The method is based on withdrawal of penis from the vagina before ejaculation.
This method has high failure rate due to pre-ejaculatory release of sperms or failure to withdraw penis from the vagina before ejaculation.
(iii) Lactational Amenorrhoea :
Just after parturition, there is a phase of amenorrhoea or absence of menstruation.
It is also the phase of intense lactation.
Breast feeding the child fully prevents conception.
The method is, however, effective only upto a maximum period of six months.
Concept Map
2. Barrier Methods :
These are mechanical devices which prevent the deposition of sperms into vagina and their passage into the uterus.
Further, they can be self inserted by the user in complete privacy.
The common barrier methods are condoms, diaphragm, fem shield and cervical cap.
(i) Condom:
It is tubular latex sheath which is rolled over the male copulatory organ during sex.
The common brand provided by family welfare services is Nirodh.
The device also provides protection against sexually transmitted diseases including AIDS.
(ii) Fem Shield (Female Condom) :
The device is polyurethane pouch with a ring at either end.
The inner ring is smaller and present at the inner closed end.
The device covers the external genitalia as well as lines the vagina.
Fem shield provides protection from sexually transmitted diseases also.
(iii) Diaphragm:
It is a tubular rubber sheath with a flexible metal or spring ring at the margin which is fitted inside the vagina.
 (iv) Cervical Cap:
(iv) Cervical Cap:

It is rubber nipple which is fitted over the cervix and is designed to remain there by suction.
The device prevents the entry of sperms into the uterus.
 (v) Vault Cap :
(v) Vault Cap :

It is hemispheric dome like rubber or plastic cap with a thick rim which is meant for fitting over the vaginal vault over the cervix.
3. Chemical Methods:
These are contraceptives which contain spermicidal chemicals.
The chemical contraceptives are available in the form of creams (e.g., delfen), jelly (perceptin, volpar paste), foam tablets (e.g., aerosol foam, chlorimin T or contab).... etc.
These commonly contain lactic acid, boric acid, citric acid, zinc sulphate and potassium permanganate.
The contraceptives are introduced in vagina prior to sex.
Sponge (Today) is a foam suppository or tablet containing nonoxynol-9 as spermicide. It kills the sperm by disrupting the membrane. It is moistened before use to activate the spermicide. The device also absorbs the male ejaculate.
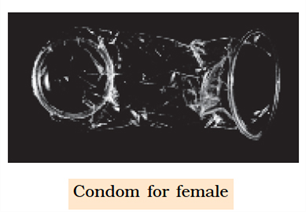
4. Intrauterine Devices (IUDs) (Intrauterine Contraceptive Devices or IUCDs) :
 These devices are inserted by doctors or expert nurses in the uterus through vagina. IUDs affect motility of sperms within the uterus. These IUDs can be –
These devices are inserted by doctors or expert nurses in the uterus through vagina. IUDs affect motility of sperms within the uterus. These IUDs can be –
(a) Non-medicated (e.g., Lippes loop)
(b) Copper releasing (e.g., CuT, Cu7, Multiload 375) – The copper ions suppress the motility and fertilization capacity of sperms.
(c) Hormone releasing (e.g., Progestasert, LNG-20)- The hormone releasing IUDs, in addition, make the uterus unsuitable for implantation and the cervix hostile to the sperms.
IUDs are ideal contraceptives for the females who want to delay pregnancy and / or space children. It is one of the most widely accepted methods of contraception in India.
5. Oral Contraceptives (Oral Pills) :
 Are preparations containing either progestin (= progestogen = progesterone) alone or a combination of progestogen and oestrogen (= estrogen).
Are preparations containing either progestin (= progestogen = progesterone) alone or a combination of progestogen and oestrogen (= estrogen).
The pills are taken orally for 21 days in a menstrual cycle starting from 5th day and ending on 25th day.
However, it is advisable to restart the course after a gap of 7 days irrespective of the onset or nonset of menstruation during the pill free days.
When a pill is missed, it should be taken whenever one remembers, sometimes two at a time.
This helps in keeping the hormonal level optimum for contraception.
Hormonal pills act by four ways :
(a) Inhibition of ovulation.
(b) Alternation in uterine endometrium to make it unsuitable for implantation.
(c) Changes in cervical mucus impairing its ability to allow passage and transport of sperms.
(d) Inhibition of motility and secretory activity of fallopian tubes.
Oral pills are of two types, combined and minipills.
Combined pills contain both oestrogen and progestin.
They are synthetic products.
Oestrogen is an ovulatory, that inhibits FSH production. Progestin is anovulatory that inhibits LH production.
It protects the endometrial lining from adverse effect of oestrogen.
The hormone also changes cervical mucus.
The most commonly used progestin is levonorgestrel or desogestrel.
The most common oestrogen is ethinyl oestradiol or menstranol.
In monophasic combined pill, both oestrogen and progestin are present in nearly the same amount, e.g., Mala D, Mala L.
In multiphasic combined pills, oestrogen is maintained at the same level throughout the 21 day course (0.03 mg). But the amount of progestin is increased (0.05 mg for first six days, 0.075 for next 5 days and 0.125 mg for last ten days), e.g., triquilar, orthonovum.
Minipills are progestin pills only (with no estrogen). They are taken daily without break.
Saheli, a nonsteroidal preparation, is taken once a week after an initial intake of twice a week dose for 3 months.
6. Injectable Contraceptives (Depo-Provara) :
Two types of progestin preparations are used singly.
They are depot-medroxy progesterone acetate (DMPA) 150 mg every three months or 300 mg every six months and norethisterone enanthate (NET EN) 200 mg every two months.
Cyclofem and mesigna and combined injectable contraceptives which are given once every month.
They contain progestin preparation as well as oestradiol.
7. Implants:
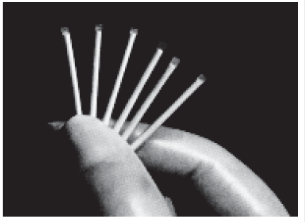
 They are hormone containing devices which are implanted subdermally for providing long term contraception.
They are hormone containing devices which are implanted subdermally for providing long term contraception.
Norplant is progestin only. The device is with six small permeable capsules (34 mm × 2.4 mm) each with about 36 mg levonorgestrel.
They are inserted under the skin in a fan shaped manner inside upper arm or fore arm through a small incision.
Suturing is not required. Norplant remains effective for about 5 years.
Implanon is a single rod-like device which is implanted through a wide bored needle. It contains 3-keto desogestrel. It remains functional for three years.
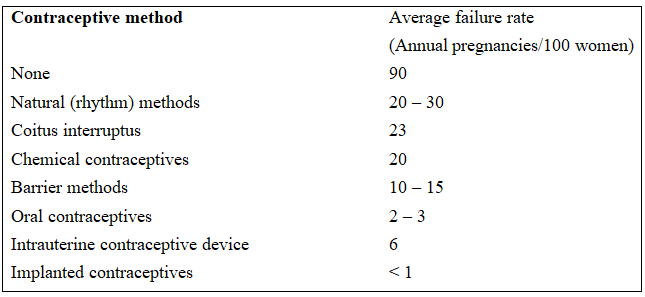
Average Failure Rate of Various Contraceptive Techniques
8. Emergency Contraception :
It is treatment for unprotected sex, sexual assault, missed pills and other reasons which have risk of pregnancy.
The drugs used for treating emergency contraceptions are called morning-after pills.
They are also available in India under Family Welfare Programme since 2002-2003.
Two ovral tablets to start and two tablets after 12 hours provide relief.
Other morning-after pills are noral, norgynon and ovidon.
An antiprogesterone pill (mifepristone) is a single pill treatment.
Insertion of IUD within five days of unprotected sex prevents implantation.
9. Surgical Methods of Family Planning :
They are also called terminal methods of family planning.
Surgical methods are permanent methods of family planning where there is no need of replacement or augmentation but the reversibility is poor.
The methods are operative procedures which block the passage of semen in males and ova in females.
The techniques are also called sterilisation procedures.
They are called vasectomy in males and tubectomy in females.
Vasectomy (L. vas-vessel, ektome-excision) :
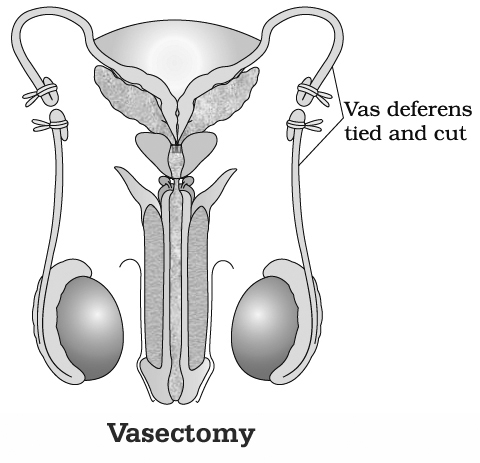
It is a surgical method of sterilisation of males.
Vasa deferentia are blocked by cutting and occluding them so that sperms are unable to pass down the male reproductive system.
(i) Conventional Vasectomy (Scalpel Surgery) :
Under local anaesthesia, transverse 1cm incision is made through the skin of the scrotum with the help of the scalpel over the area of vasa deferentia.
Each vas deferense is exposed and cut.
The two ends are separated and tied.
A gap of 1-4cm is must between the two ends otherwise reunion can occur.
(ii) No-scalpel Vasectomy:
Here instead of scalpel, a dissecting forceps and a ringed forceps are required.
The skin is punctured and the vas deferense is taken out.
It is occluded by removal of 1-2 cm followed by ligation of ends.
Occlusion can also be achieved by heat and clips.
Vasectomy is a reversible procedure as the cut ends can be joined together to open to sperm passage.
Tubectomy (L. tubes-pipe, ektome-excision):
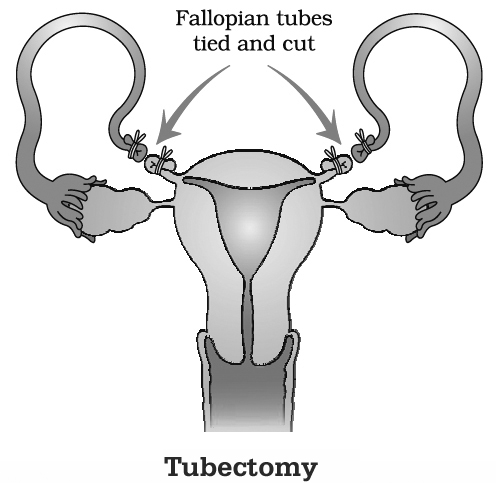
It is a surgical procedure of female sterilisation where a portion of both the fallopian tubes is excised or ligated to block the passage of ovum through them.
Tubectomy is performed by conventional transabdominal surgery, conventional laparotomy and minilaparotomy.
In surgical procedures, the fallopian tubes are cut and the cut ends are tied to prevent reunion.
The procedure is reversible as the cut ends can be rejoined.
In laparoscopic procedure, sterlisation is achieved by loop development and constricting the basal region of loop with the help of elastic ring either through a small incision in the abdomen or through vagina.
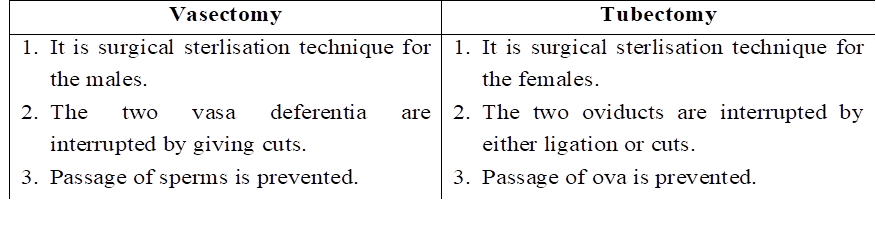
Difference between Vasectomy and Tubectomy
Medical Termination of Pregnancy (MTP)
It is voluntary or intentional abortion induced and performed to end pregnancy before the completion of full term.
Worldwide, nearly 20% of the total pregnancies get aborted.
The number of MTPs is 40-50 million/yr.
Therefore, MTPs have a significant role in containment of population though they are not performed for this purpose.
They are mainly meant for removing unsustainable pregnancies.
Many countries do not have a law about MTPs because the latter involve emotional, ethical, religious and social issues.
However, in India there is a proper act, Medical Termination of pregnancy Act, 1971.
It is mainly meant for preventing unnatural maternal deaths due to unsafe abortions (8.9% of the total maternal deaths).
The act has been amended in 2002.
Under this act termination of pregnancy can be done upto 20 weeks, if pregnancy is likely to produce a congenitally malformed child, is a result of rape and contraceptive failure or is likely to harm the mother.
MTP is safe if it is performed upto 12 weeks (first trimester) of pregnancy.
Misoprostol (prostaglandin) alongwith mifepristone (antiprogesterone) is an effective combination.
Vacuum aspiration and surgical procedures are adopted thereafter.
Second trimester abortions are risky.
They are generally performed after testing the sex of the baby through amniocentesis or sonography.
It has resulted in large scale female foeticide and complications due to unsafe abortions in the hands of untrained persons.
To prevent such happening, the government has enacted a law, Pre-natal diagnostic techniques (Regulation and Prevention of Misuse) Act, 1994 with amendments in 2003.
It prohibits preconception and prenatal sex determination.
 ACME SMART PUBLICATION
ACME SMART PUBLICATION
