Concepts of Abnormality and Psychological Disorders
- Books Name
- Psychology Book Class-12
- Publication
- PathSet Publications
- Course
- CBSE Class 12
- Subject
- Psychology
Concepts of Abnormality and Psychological Disorders
Psychological disorders are: (Four D’s)
- Deviant (different, extreme, unusual, bizarre)
- Distressing (unpleasant and upsetting to the person and to others)
- Dysfunctional (interfering with the person’s ability to carry out daily activities in a constructive way)
- Dangerous (to the person or to others)
‘Abnormal’ literally means “away from the normal”, it implies deviation from some clearly defined norms or standards.
Approaches to distinguish between normal and abnormal behavior:
The first approach views abnormal behavior as a deviation from social norms.
- According to this approach, ‘Abnormal’ is simply a label that is given to a behavior which is deviant from social expectations.
- Abnormal behavior, thoughts and emotions are those that differ markedly from a society’s ideas of proper functioning.
- Each society has norms, which are stated or unstated rules for proper conduct. Behaviors, thoughts and emotions that break societal norms are called abnormal.
- A society’s norms grow from its population culture - its history, values, institutions, habits, skills, arts and technology.
- A society’s values may change over time, causing its view of what is psychologically abnormal to change as well.
- Socially accepted behavior is not abnormal, and normality is nothing more than conformity to social norms.
The second approach views abnormal behavior as maladaptive.
- According to this approach, the best criterion for determining the normality of behavior is not whether the society accepts it but whether it fosters the well-being of the individual and eventually of the group to which he/she belongs.
- Well-being is simply not maintenance and survival but also includes growth and fulfilment i.e. the actualization of potential.
- Conforming behavior can be seen as abnormal if it is maladaptive, i.e. if it interferes with optimal functioning and growth.
- Describing behavior as maladaptive implies that a problem exists; it also suggests that vulnerability in the individual, inability to cope, or exceptional stress in the environment have led to problems in life.
Historical Background
- Books Name
- Psychology Book Class-12
- Publication
- PathSet Publications
- Course
- CBSE Class 12
- Subject
- Psychology
Historical Background
Supernatural Approach
- Abnormal behavior can be explained by the operation of supernatural and magical forces such as evil spirits or the devil.
- Exorcism i.e. removing the evil that resides in the individual through countermagic and prayer, is still commonly used.
- In many societies, the shaman, or medicine man (ojha) is a person who is believed to have a contact with supernatural forces and is the medium through which spirits communicate with human beings. Through the shaman, and afflicted person can learn which spirts are responsible for his/her problems and what needs to be done to appease them.
- Biological or Organic Approach
- Individuals behave strangely because their bodies and their brains are not working properly is another belief in the history of abnormal psychology.
- Body and brain processes have been linked to many types of maladaptive behaviors.
- For certain types of disorders, correcting these defective biological processes results in improved functioning.
Psychological Approach
- According to this, psychological problems are caused by inadequacies in the way an individual thinks, feels or perceives the world.
Organismic Approach
- Hippocrates, Socrates and in particular Plato (philosopher-physicians of ancient Greece) viewed disturbed behavior as arising out of conflicts between emotion and reason.
Based on Four Humours
- Galen elaborated on the role of four humors in personal character and temperament.
- According to him, the material world was made up of four elements (earth, air, fire and water) which combine to form four essential body fluids (blood, black bile, yellow bile and phlegm).
- Each of these fluids was seen to be responsible for a different temperament.
- Imbalances among the humours were believed to cause various disorders.
In Middle Ages
- Demonology and superstition gained renewed importance in the explanation of abnormal behavior.
- Demonology related to a belief that people with mental problems were evil and there are numerous instances of ‘witch-hunt’ during this period.
- During the early Middle Ages, the Christian spirit of charity prevailed and St. Augustine wrote extensively about feelings, mental anguish and conflict.
- This laid the groundwork for modern psychodynamic theories of abnormal behavior.
Renaissance Period
- This period was marked by increased humanism and curiosity about behavior.
- Johann Weyer emphasized psychological conflict and disturbed interpersonal relationships as causes of psychological disorders.
- He also insisted that ‘witches’ were mentally disturbed and required medical, not theological, treatment.
Age of Reason and Enlightenment (17th & 18th century)
- The scientific method replaced faith and dogma as ways of understanding abnormal behavior.
- The growth of a scientific attitude towards psychological disorders in the 18th century contributed to the Reform Movement and to increased compassion for people who suffered from these disorders.
- Reforms of asylums were initiated both in Europe and America.
- One aspect of the reform movement was the new inclination for deinstitutionalization which placed emphasis on providing community care for recovered mentally ill individuals.
Interactional or Bio-Psycho-Social Approach
- From this perspective, all three factors (biological, psychological and social) play important role in influencing the expression and outcome of psychological disorders.
Classification of Psychological Disorders
- Books Name
- Psychology Book Class-12
- Publication
- PathSet Publications
- Course
- CBSE Class 12
- Subject
- Psychology
Classification Of Psychological Disorders
- A classification of psychological disorders consists of a list of categories of specific psychological disorders grouped into various classes on the basis of some shared characteristics.
- Classifications are useful because they enable users like psychologists, psychiatrists and social workers to:
- Communicate with each other about the disorder
- Help in understanding the causes of psychological disorders and the processes involved in their development and maintenance
- Official manuals describing and classifying various kinds of psychological disorders:
1) Diagnostic and Statistical Manual of Mental Disorders 5th Edition (DSM-5): Current
by the American Psychiatric Association (APA)
It presents discrete clinical criteria which indicate the presence or absence of disorders.
2) International Classifications of Diseases (ICD-10)
ICD-10 Classification of Behavioral and Mental Disorders by WHO (World Health Organizations)
For each disorder, a description of the main clinical features or symptoms, and of other associated features including diagnostic guidelines is provided.
Factors Underlying Abnormal Behaviour
- Books Name
- Psychology Book Class-12
- Publication
- PathSet Publications
- Course
- CBSE Class 12
- Subject
- Psychology
Factors Underlying Abnormal Behavior
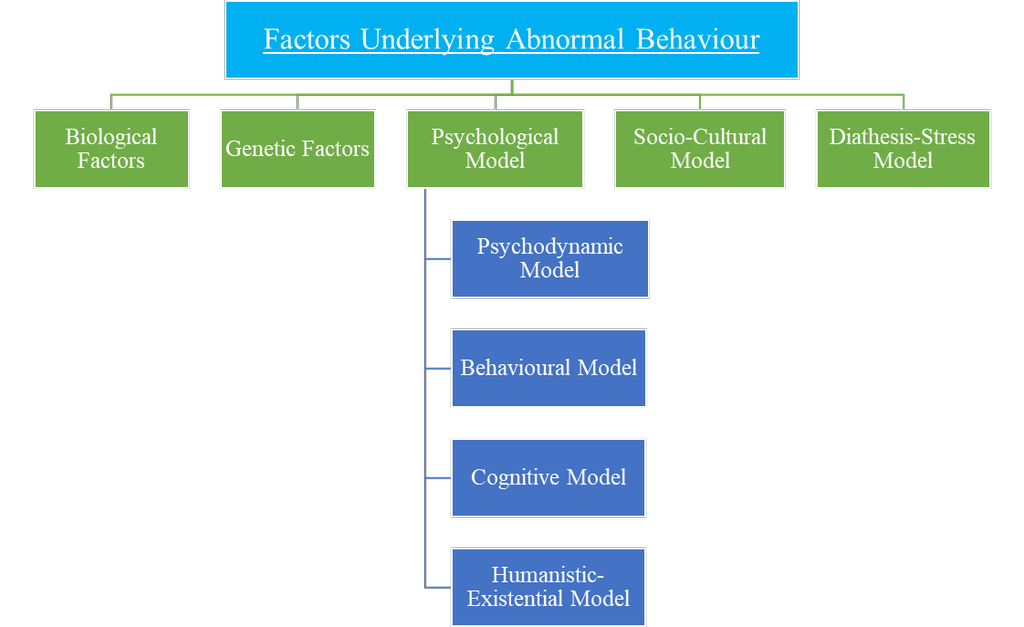
Biological Factors influence all aspects of our behavior.
- A wide range of biological factors may interfere with normal development and functioning of the human body such as:
- Faulty genes
- Endocrine imbalances
- Malnutrition
- Injuries
- These factors may be potential causes of abnormal behavior.
- According to the biological model, abnormal behavior has a biochemical or physiological basis.
- Psychological disorders are often related to problems in the transmission of messages from one neuron to another across synapse.
- When an electrical impulse reaches a neuron’s ending, the nerve ending is stimulated to release a chemical called neuro-transmitter.
- Abnormal activity by certain neuro-transmitters can lead to specific psychological disorders. For example,
- Anxiety disorders have been linked to low activity of neurotransmitter - gamma aminobutyric acid (GABA)
- Schizophrenia to excess activity of dopamine.
- Depression to low activity of serotonin.
Genetic Factors
- They have been linked to mood disorders, schizophrenia, mental retardation and other psychological disorders such as depression, anxiety, etc.
- In most cases, no single gene is responsible for a particular behaviour or a psychological disorder. In fact, many genes combine to help bring about our various behaviours and emotional reactions, both functional and dysfunctional.
Psychological Model
- This model also provides a psychological explanation of mental disorders.
- These models maintain that psychological and interpersonal factors have a significant role to play in abnormal behavior.
- These factors include:
(a) Maternal deprivation
- Separation from the mother
- Lack of warmth and stimulation during early years of life.
(b) Faulty parent-child relationships
- Rejection
- Overprotection
- Over-permissiveness
- Faulty discipline
(c) Maladaptive family structures
- Inadequate or disturbed family
(d) Severe stress
Psychodynamic Model (oldest and most famous of the modern psychological models)
- Theorists believe that behaviour, whether normal or abnormal, is determined by psychological forces within the person of which she/he is not consciously aware.
- These internal forces are considered dynamic i.e. they interact with one another and their interaction gives shape to behaviours, thoughts and emotions.
- Abnormal symptoms are viewed as the result of conflicts between these forces.
- Freud believed that 3 central forces shape personality:
- Instinctual needs, drives and impulses (id)
- Rational thinking (ego)
- Moral standards (super ego)
- He stated that abnormal behavior is a symbolic expression of unconscious mental conflicts that can be generally traced to early childhood or infancy.
Behavioral Model
- It states that both normal and abnormal behaviors are learned and psychological disorders are the result of learning maladaptive ways of behaving.
- It concentrates on behaviors that are learned through conditioning and propose that what has been learned can be unlearned.
- Learning can take place by:
- Classical conditioning (temporal association in which two events repeatedly occur close together in time)
- Operant conditioning (behavior is followed by a reward)
- Social learning (learning by imitating others’ behavior)
- These 3 types of conditioning account for behavior, whether adaptive or maladaptive.
Cognitive Model
- It states that abnormal functioning can result from cognitive problems.
- People may hold assumptions and attitudes about themselves that are irrational and inaccurate.
- People may also think repeatedly in illogical ways and make overgeneralizations i.e. they may draw broad, negative conclusions on the basis of a single insignificant event.
Humanistic-Existential Model
- Focuses on broader aspects of human existence.
- Humanists believe that human beings are born with a natural tendency to be:
- Friendly
- Cooperative
- Constructive
- Are driven to self-actualize i.e. to fulfill this potential for goodness and growth
- Existentialists believe that from birth we have total freedom to give meaning to our existence or to avoid that responsibility
- Those who shrink from this responsibility would like
- Empty
- Inauthentic and
- Dysfunctional lives
Socio-Cultural Model
- Socio cultural factors such as:
- War and violence
- Group prejudice and discrimination
- Economic and employment problems
- Rapid social change
put stress on most of us and can also lead to psychological problems in some individuals.
- According to this model, abnormal behavior is best understood in light of the social and cultural forces that influence an individual.
- As behavior is shaped by societal forces, following factors become more important:
a) Family structure and communication
Certain family systems are likely to produce abnormal functioning in individual members.
Some families have an enmeshed structure in which the members are overinvolved in each other’s activities, thoughts and feelings. Children from this kind of family may have difficulty in becoming independent in life.
b) Social networks
The broader social networks in which people operate include their social and professional relationships.
People who are isolated and lack social support, i.e., strong and fulfilling interpersonal relationships in their lives are likely to become more depressed and remain depressed longer than those who have good friendships.
c) Societal labels and roles
Abnormal functioning is influenced by the societal labels and roles assigned to troubled people. When people break the norms of their society, they are called deviant and ‘Mentally ill’.
- Such labels tend to stick so that the person may be viewed as ‘crazy’ and encouraged to act sick. The person gradually learns to accept and play the sick role, and functions in a disturbed manner.
Diathesis - Stress Model (widely accepted)
- It states that psychological disorders develop when a diathesis (biological predisposition to the disorder) is set off by a stressful situation.
- This model has 3 components:
- The first is the diathesis or the presence of some biological aberration which may be inherited.
- The second is that the diathesis may carry a vulnerability to develop a psychological disorder. This means that the person is ‘at risk’ or ‘predisposed’ to develop the disorder.
- The third is the presence of pathogenic stressors, i.e. factors/stressors that may lead to psychopathology.
- If such "at risk" persons are exposed to these stressors, their predisposition may actually evolve into a disorder.
- This model has been applied to several disorders including anxiety, depression and schizophrenia.
Major Psychological Disorders
- Books Name
- Psychology Book Class-12
- Publication
- PathSet Publications
- Course
- CBSE Class 12
- Subject
- Psychology
Major Psychological Disorders
1) Anxiety Disorders
- High levels of anxiety that are distressing and interfering with effective functioning indicate the presence of an anxiety disorder.
- The term 'anxiety' is usually defined as a diffuse, vague, very unpleasant feeling of fear and apprehension.
- The anxious individual shows combinations of the following symptoms:
- Rapid heart rate
- Shortness of breath
- Diarrhea
- Loss of appetite
- Fainting
- Dizziness
- Sweating
- Sleeplessness
- Frequent urination
- Tremors
a) Generalized Anxiety Disorder
- Consists of prolonged, vague, unexplained and intense fears that are not attached to any particular object.
- Symptoms:
- Worry and apprehensive feelings about the future
- Hypervigilance (involves constantly scanning the environment for dangers)
- Motor tension, as a result of which the person is unable to relax, is restless and visibly shaky and tense.
b) Panic Disorder
- Consists of recurrent/frequent anxiety attacks in which the person experiences intense terror and dread.
- A panic attack denotes an abrupt surge of intense anxiety rising to a peak when thoughts of a particular stimuli are present.
- Such thoughts occur in an unpredictable manner.
- Clinical features:
- Shortness of breath
- Dizziness
- Chest pain or discomfort
- Palpitations
- Fear of going crazy
- Nausea
- Choking
- Losing control
- Dying
- Trembling
c) Phobias
- Irrational fears related to specific objects, people or situations.
- They develop gradually or begin with a generalized anxiety disorder.
- Phobias can be grouped into three main types, i.e. specific phobias, social phobias, and agoraphobia.
(i) Specific Phobias
- Most commonly occurring type of phobia
- Irrational fears such as:
- Intense fear of a certain type of animal
- Being in an enclosed space.
(ii) Social Phobias
- Intense and incapacitating fear and embarrassment when dealing with others.
- Also known as Social Anxiety Disorder
(iii) Agoraphobia
- When people develop a fear of entering unfamiliar situations
- Many agoraphobics are:
- Afraid of leaving their home
- Unable to carry out normal life activities
d) Separation Anxiety Disorders
- Individuals are fearful and anxious about separation from attachment figures to an extent that is developmentally not appropriate.
- Extreme distress when expecting or going through separation from home or other significant people to whom the individual is immensely attached to.
- Children with SAD may have difficulty:
- Being in a room by themselves
- Going to school alone
- Are fearful of entering new situations
- Cling to and shadow their parents’ every move
- To avoid separation, children with SAD may:
- Fuss
- Scream
- Throw severe tantrums
- Make suicidal gestures
e) Other disorders are:
- Selective Mutism
- Substance/Medication Induced Anxiety Disorder
- Anxiety Disorder due to another medical condition
2) Obsessive - Compulsive and Related Disorders
a) Obsessive - Compulsive Disorder (OCD)
- People affected by OCD are unable to control their preoccupation with specific ideas.
- Unable to prevent themselves from repeatedly carrying out a particular act or series of acts that affect their ability to carry out normal activities.
- Obsessive behavior is the inability to stop thinking about a particular idea or topic which the person involved often finds to be unpleasant and shameful.
- Compulsive behavior is the need to perform certain behaviors over and over again.
- Example- counting, ordering, checking, touching, washing.
b) Other disorders are:
- Hoarding disorder
- Trichotillomania (hair-pulling disorder)
- Excoriation (skin-picking disorder)
3) Trauma and stressor related disorders
a) Post-traumatic stress disorder (PTSD)
- People who experience PTSD are often the ones:
- Caught in a natural disaster
- Have been victims of bomb blasts by terrorists
- Been in a serious accident
- Been in a war-related situation
- Symptoms vary widely but may include:
- Recurrent dreams
- Flashbacks
- Impaired concentration
- Emotional numbing
b) Other disorders are:
- Adjustment disorders
- Acute stress disorder
4) Somatic Symptom and Related Disorders
- People experience physical symptoms in the absence of a physical disease.
- The individual has psychological difficulties and complains of physical symptoms, for which there is no biological cause.
a) Somatic Symptom Disorder (presence of physical complaints)
- involves a person having persistent body-related symptoms which may or may not be related to any serious medical condition.
- People with this order tend to be overly preoccupied with their symptoms.
- Continually worry about their health.
- Make frequent visits to doctor
- As a result, they experience significant distress and disturbances in their daily life.
b) Illness Anxiety Disorder (presence of anxiety)
- Involves persistent preoccupation about developing a serious illness and constantly worrying about their possibility
- Accompanied by anxiety about one’s health.
- People with this disorder are overly concerned about undiagnosed disease and negative diagnostic results.
- Do not respond to assurance by doctors
- Are easily alarmed about illness such as on hearing about someone else’s ill-health or some such news.
c) Conversion Disorders
- The symptoms of conversion disorders are the reported loss of part or all of some basic body functions for example:
- Paralysis
- Blindness
- Deafness
- Difficulty in walking
- These symptoms often occur after a stressful experience and may be quite sudden, and have no physical cause.
5) Dissociative Disorders
- Dissociation can be viewed as severance of the connections between ideas and emotions.
- It involves feelings of:
- Unreality
- Depersonalisation
- Estrangement
- Sometimes a loss or shift of identity
- Characteristic:
- Sudden temporary alterations of consciousness that blot out painful experiences.
a) Dissociative Amnesia
- Extensive but selective memory loss that has no known organic cause (example- head injury)
- Some people cannot remember anything about their past
- Others can no longer recall specific events, people, places or objects, while their memory for other events remain intact.
- A part of dissociative amnesia is dissociative fugue.
- Essential features of dissociative fugue are:
- Unexpected travel away from home and workplace
- Assumption of a new identity
- Inability to recall the previous identity
- The fugue usually ends when the person suddenly ‘wakes up’ with no memory of the events that occurred during the fugue.
- This disorder is often associated with an overwhelming stress.
b) Dissociative Identity Disorder (referred to as ‘multiple personality’)
- Most dramatic
- Often associated with traumatic experiences in childhood
- The person assumes alternate personalities that may or may not be aware of each other
c) Depersonalization/Derealization Disorder
- Involves a dream-like state in which the person has a sense of being separated both from self and from reality
- In depersonalization, there is a change of self-perception and the person’s sense of reality is temporarily lost or changed.
6) Depressive Disorders
- Depression is one of the most widely prevalent and recognized of all mental disorders.
- It covers a variety of negative mood and behavioral changes.
- It can be referred to as a symptom as well as a disorder.
a) Major Depressive Disorder
(i) A period of:
- Depressed mood
- Loss of interest or pleasure in most activities
- Change in body weight
- Constant sleep problems
- Tiredness
- Inability to think clearly
- Agitation
- Greatly slowed behavior
- Thoughts of death and suicide
- Excessive guilt
- Feelings of worthlessness
(ii) Factors predisposing towards depression (Risk factors):
- Genetic make-up/ heredity
- Age
- Women during young adulthood
- Men during early middle age
- Gender
- Women are more likely to report a depressive disorder
- Negative life event
- Lack of social support
7) Bipolar And Related Disorders
a) Bipolar I Disorder (earlier referred to as ‘Manic- depressive disorders’)
- Involves mania and depression, which are alternatively present and sometimes interrupted by periods of normal mood.
- Manic episodes rarely appear by themselves; they usually alternate with depression.
b) Other disorders are:
- Bipolar II disorder
- Cyclothymic disorder
Suicide
- Can take place at any point of time of life
- Result of complex interface of biological, genetic, psychological, sociological, cultural and environmental factors.
- Risk factors are:
- Having mental disorders (especially depression and alcohol use disorders)
- Going through natural disasters
- Experiencing violence, abuse or loss
- Isolation at any stage of life
- Previous suicidal attempt (Strongest risk factor)
- Suicidal behavior often indicates difficulties in:
- Problem-solving
- Stress management
- Emotional expression
- Suicidal thoughts lead to suicidal action only when acting on these thoughts seems to be the only way out of a person’s difficulties
- These thoughts are heightened under acute emotional and other distress
- The ramifications of suicide on social circle and communities tend to be devasting and long-lasting.
- The stigma surrounding suicide compel many people, who are contemplating or even attempting suicide, to not seek help thus, preventing timely help from reaching them.
- Therefore, improving identification, referral and management of behavior are crucial for preventing suicide.
- Therefore, we need to:
- Identify the vulnerability
- Comprehend the circumstances leading to such behavior
- Accordingly plan interventions
- Suicides are preventable but there is a need for comprehensive multi-sectoral approach where the government, media and civil society all play important role as stake holders.
- Measures suggested by WHO for preventing suicides are:
- Limiting access to the means of suicide.
- Reporting of suicide by media in a responsible way
- Bringing in alcohol related policies
- Early identification, treatment and care of people at risk
- Training health workers in assessing and managing for suicide
- Care for people who attempted suicide and providing community support.
Identifying Students In Distress
- Any unexpected or striking change affecting the adolescent’s performance, attendance or behavior should be taken seriously, such as:
- Lack of interest in common activities
- Declining grades
- Decreasing effort
- Misbehavior in the classroom
- Mysterious or repeated absence
- Smoking or drinking, or drug misuse.
Strengthening Students’ Self Esteem
- Having a positive self-esteem is important in face of distress and helps in coping adequately.
- In order to foster positive self-esteem in children the following approaches can be useful:
- Accentuating positive life experiences to develop positive identity leading to increased confidence in self.
- Providing opportunities for development of physical, social and vocational skills
- Establishing a trustful communication
- Goals for the students should be specific, measurable, achievable, relevant, to be completed within a relevant time frame.
8) Schizophrenia Spectrum and Other Psychotic Disorders
- Schizophrenia is a descriptive term for a group of psychotic disorders in which personal, social and occupational functioning deteriorate as a result of disturbed thought processes, strange perceptions, unusual emotional states, and motor abnormalities.
- Debilitating disorder
- The social and psychological costs of schizophrenia are tremendous, both to patients as well as to their families and society.
- Symptoms of schizophrenia:
a) Positive symptoms (i.e., excesses of thought, emotion and behavior)
‘Pathological excesses’ or ‘bizarre additions’ to a person’s behavior
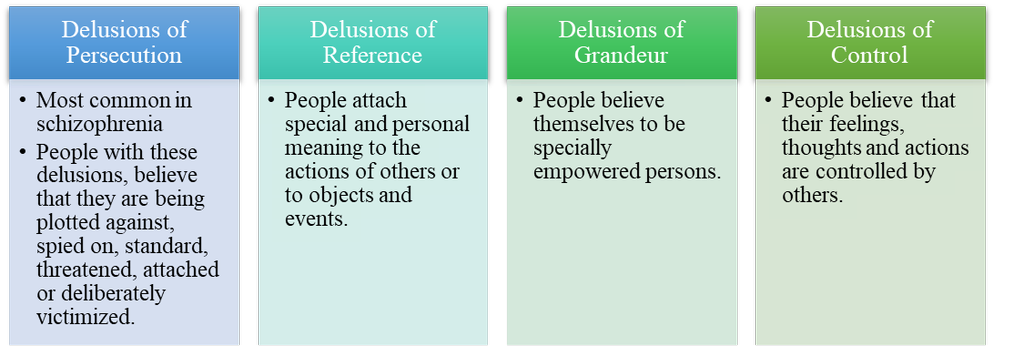
Delusions
- A delusion is a false belief that is firmly held on inadequate grounds.
- It is not affected by rational argument.
- It has no basis in reality
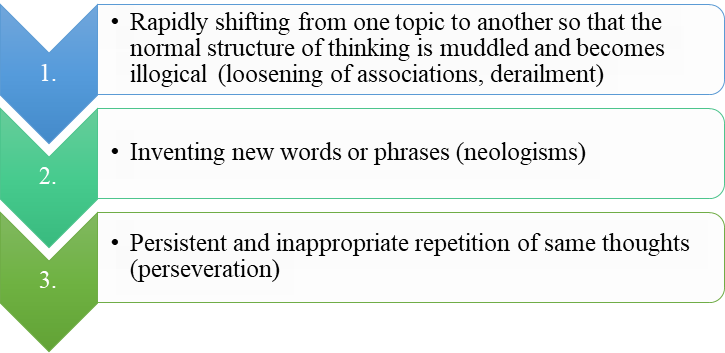
Disorganized thinking and speech/ Formal thought disorders
- May not be able to think logically
- May speak in peculiar ways
- Make communication extremely difficult
- Includes:
Heightened perception and Hallucinations
- They are perceptions that occur in the absence of external stimulus.
- Inappropriate affect i.e. emotions that are unsuited to the situation
b) Negative symptoms (i.e. deficits of thought, emotion and behavior)
‘Pathological Deficits’
Alogia or Poverty of speech
- Reduction in speech and speech content
Blunted Affect
- Show less anger, sadness, joy and other feelings than most people do
Flat Affect
- Some show no emotions at all
Avolition/ Apathy (lack of interest, enthusiasm or concern)
- Inability to start or complete a course of action
Social Withdrawal
- May withdraw socially and become tally focused on their own ideas and fantasies
Psychomotor Symptoms
- move less spontaneously
- make odd grimaces and gestures
- may take extreme forms known as catatonia
- People in a catatonic stupor remain motionless and silent for long stretches of time.
- Catatonic rigidity i.e., mainting a rigid, up bright posture for hours.
- Catatonic posturing i.e., assuming awkward, bizarre positions for long periods of time.
9) Neurodevelopmental Disorders
- Common feature - they manifest in the early stage of development
- The symptoms often appear before the child enters school or during the early stage of schooling
- These disorders result in:
- Hampering personal, social, academic and occupational functioning.
- Characteristics:
- Deficits or excesses in a particular behavior
- Delays in achieving a particular age-appropriate behavior
10) Attention Deficit/Hyperactivity Disorder (ADHD)
- If not attended, can lead to more serious and chronic disorders as the child moves into adulthood.
- Main features are:
a) Inattention
- Children find it difficult to sustain mental effort during work or play.
- Have a hard time keeping their minds on any one thing
- Have a hard time in following instructions:
- Common complaints are:
- Child does not listen
- Cannot concentrate
- Does not follow instructions
- Is disorganized
- Easily distracted
- Forgetful
- Does not finish assignments
- Quick to lose interest in boring activities
b) Impulsivity
- Children seem unable to control their immediate reactions
- Unable to think before they act
- Find it difficult to wait or take turns
- Have difficulty resisting immediate temptations or delaying gratification
- Minor mishaps such as knocking things over are common, whereas more serious accidents and injuries can also occur.
c) Hyperactivity
- Children are in constant motion
- Sitting still through a lesson is impossible for them
- Child may fidget, squirm, climb and run around the room aimlessly
- Parents and teachers describe them as ‘driven by a motto’, always on the go, and talk incessantly.
11) Autism Spectrum Disorder (ASD)
- If not attended, can lead to more serious and chronic disorders as the child moves into adulthood.
- Characteristics:
- Widespread impairments in social interaction and communication skills.
- Stereotyped patterns of behaviors, interests and activities.
- Children with ASD have:
- Marked difficulties in social interaction and communication across different contexts
- A restricted range of interests
- Strong desire for routine
- About 70% of children with ASD have intellectual disabilities.
- Children with ASD:
- Experience profound difficulties in relating to other people.
- Are unable to initiate social behavior
- Seem unresponsive to other people’s feelings
- Unable to share experiences or emotions with others
- Show serious abnormalities in communication and language that persist over time
- Many of them never develop speech and those who do, have repetitive and deviant speech patterns
- Show narrow patterns of interests
- Show repetitive behaviors such as lining up objects or stereotyped body movements such as rocking.
- These motor movements may be:
- Self-stimulatory such as hand flapping
- Self-injurious such as banging their heads against the wall.
- Tend to experience difficulties in starting, maintaining and even understanding relationships due to the difficulties in terms of verbal and non-verbal communications.
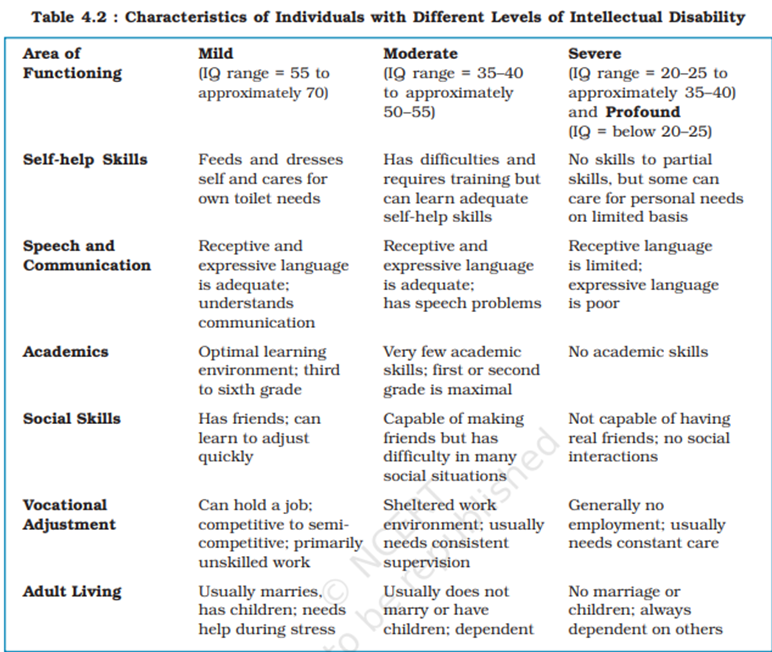
12) Intellectual Disability
- Refers to below average intellectual functioning (with an IQ of approx 70 or below)
- Deficits or impairments in adaptive behaviors (i.e. in the areas of communication, self-care, home-living, social/interpersonal skills, functional academic skills, work, etc.) which are manifested before the age of 18 years.
- If not attended, can lead to more serious and chronic disorders as the child moves into adulthood.
13) Specific Learning Disorder
- Individual experiences difficulty in perceiving or processing information efficiently and accurately.
- These get manifested during early school years.
- The individual encounters problems in basic skills in reading, writing and mathematics.
- Tends to perform below average for his/her age.
- However, with additional inputs and efforts the individuals may be able to reach acceptable performance levels.
- Likely to impair functioning and performance in activities/occupations dependent on the related skills.
- If not attended, can lead to serious and chronic disorders as the child moves into adulthood.
14) Disruptive, Impulse-Control and Conduct Disorders
a) Oppositional Defiant Disorder (ODD)
- Children display age-inappropriate amounts of stubbornness
- Are irritable, defiant, disobedient
- Behave in a hostile manner
- Do not see themselves as angry, oppositional or defiant and often justify their behavior as reaction to circumstances/demands.
- The symptoms of the disorder become entangled with problematic interactions with others.
b) Conduct Disorder/Antisocial Behaviour
- Refers to age-inappropriate actions and attitudes that violate family expectations, societal norms and personal or property right of others.
- Behaviors typical of conduct disorder include:
- Aggressive actions that cause or threaten harm to people or animals
- Non-aggressive conduct that causes property damage
- Major deceitfulness or theft
- Serious rule violations
- Children show many different types of aggressive behavior such as:
- Verbal aggression (i.e., name-calling, swearing)
- Physical aggression (i.e., hitting, fighting)
- Hostile aggression (i.e., directed at inflicting injury to others)
- Proactive aggression (i.e., dominating and bullying others without provocation)
15) Feeding And Eating Disorders
a) Anorexia Nervosa
- The individual has a distorted body image that leads her/him to see herself/himself as overweight.
- Often refuses to eat
- Exercises compulsively
- Developing unusual habits such as refusing to eat in front of others
- Person may lose large amounts of weight and even starve her/himself to death.
b) Bulimia Nervosa
- The individual may eat excessive amounts of food, then purge her/his body of food by using medicines such as laxatives or diuretics or by vomiting.
- The person often feels disgusted and ashamed when she/he binges and is relieved of tension and negative emotions after purging.
c) Binge Eating
- Frequent episodes of out-of-control eating.
- The individual tends to eat at a higher speed than normal and continues eating till she/he feels uncomfortably full.
- Large amount of food may be eaten even when the person is not feeling hungry.
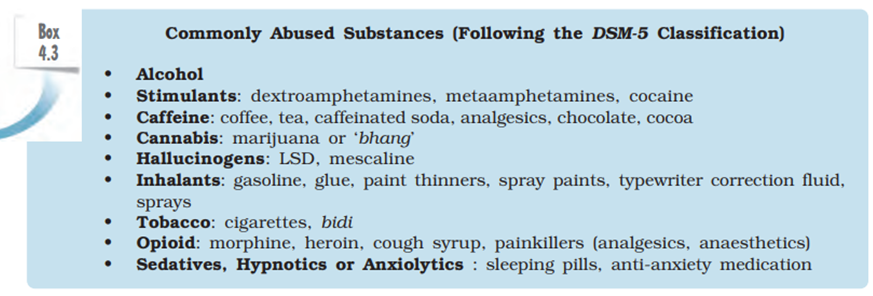
16) Substance-Related And Addictive Disorders
- Related to maladaptive behaviors resulting from regular and consistent use of the substance involved.
- Includes problems associated with the use and abuse of alcohol, cocaine, tobacco and opiods among others, which alter the way people think, feel and behave.
- Frequently used substances are:
1) Alcohol
- People who abuse alcohol, drink large amounts regularly and rely on it to help them face difficult situations.
- Eventually, the drinking interferes with their social behavior and ability to think and work.
- Their bodies build up to a tolerance for alcohol and they need to drink even greater amounts to feel its effects.
- They also experience withdrawal responses when they stop drinking.
- Alcoholism destroys:
- Millions of families
- Social relationships
- Careers
- Intoxicated drivers are responsible for many road accidents.
- Has serious effects on the children of persons with this disorder as they have higher rates of psychological problems
a) Anxiety
b) Depression
c) Phobias
d) Substance-related disorders
- Excessive drinking can seriously damage physical health.
2) Heroin
- Its intake significantly interferes with social and occupational functioning.
- Most abusers further develop a dependence on heroin, revolving their lives around the substances, building up a tolerance for it and experiencing a withdrawal reaction when they stop taking it.
- Most direct danger of heroin abuse is an overdose, which slows down the respiratory centres in the brain, almost paralyzing breathing, and in many cases causing death.
3) Cocaine
- Regular use of cocaine may lead to a pattern of abuse in which the person may be intoxicated throughout the day and function poorly in social relationships and at work.
- May also cause problems in short-term memory and attention.
- Dependence may develop, so that cocaine dominates the person’s life, more of the drug is needed to get the desired effects, and stopping it results in feeling of
a) Depression
b) Sleep problems
c) Anxiety
d) Fatigue
e) Irritability
- Cocaine poses serious dangers as it has dangerous effects on psychological functioning and physical well-being.
Nature and Process of Psychotherapy
- Books Name
- Psychology Book Class-12
- Publication
- PathSet Publications
- Course
- CBSE Class 12
- Subject
- Psychology
Nature and Process of Psychotherapy
- Psychotherapy is a voluntary relationship between the one seeking treatment (client) and the one who treats (therapist).
- The purpose of the relationship is to help the client to solve the psychological problems being faced by her/him.
- The relationship is conducive for building the trust of the client so that problems may be freely discussed.
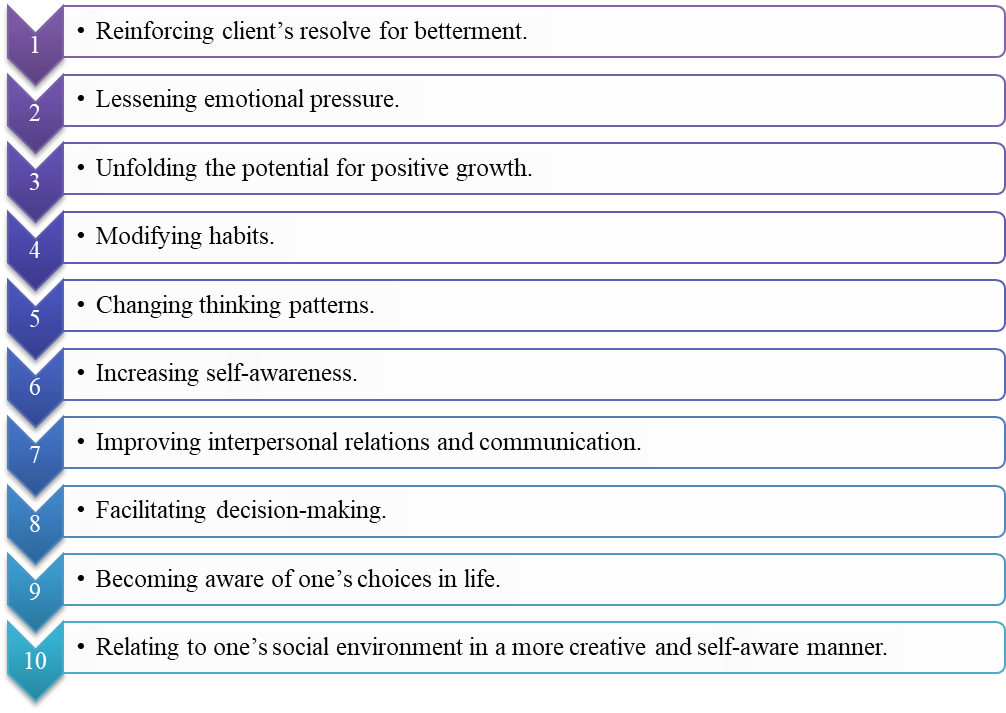
- Psychotherapies aim at:
- changing the maladaptive behaviours
- decreasing the sense of personal distress
- helping the client to adapt better to her/his environment
- Inadequate marital, occupational and social adjustment also requires that major changes be made in an individual’s personal environment.
- Characteristics of Psychotherapeutic Approaches:
- there is systematic application of principles underlying the different theories of therapy
- persons who have received practical training under expert supervision can practice psychotherapy, and not everybody. An untrained person may unintentionally cause more harm than any good
- the therapeutic situation involves a therapist and a client who seeks and receives help for her/his emotional problems (this person is the focus of attention in the therapeutic process)
- the interaction of these two persons — the therapist and the client — results in the consolidation/formation of the therapeutic relationship. This is a confidential, interpersonal, and dynamic relationship. This human relationship is central to any sort of psychological therapy and is the vehicle for change.
- Goals of Psychotherapy:
- Therapeutic Relationship or Alliance
- The special relationship between the client and the therapist is known as the therapeutic relationship or alliance.
- It is neither a passing acquaintance, nor a permanent and lasting relationship.
- Two major components of a therapeutic alliance are:
- The contractual nature of the relationship in which two willing individuals, the client and the therapist, enter into a partnership which aims at helping the client overcome her/his problems.
- The limited duration of the therapy. This alliance lasts until the client becomes able to deal with her/his problems and take control of her/ his life.
- Several unique properties of the realtionship are:
- It is a trusting and confiding relationship. The high level of trust enables the client to unburden herself/himself to the therapist and confide her/his psychological and personal problems to the latter.
- The therapist encourages this by being accepting, empathic, genuine and warm to the client.
- The therapist conveys by her/his words and behaviours that s/he is not judging the client and will continue to show the same positive feelings towards the client even if the client is rude or confides all the ‘wrong’ things that s/he may have done or thought about. This is the unconditional positive regard which the therapist has for the client (such as acceptance and respect).
- The therapist has empathy for the client. Empathy is different from sympathy and intellectual understanding of another person’s situation.
- In sympathy, one has compassion and pity towards the suffering of another but is not able to feel like the other person.
- Intellectual understanding is cold in the sense that the person is unable to feel like the other person and does not feel sympathy either.
- Empathy is present when one is able to understand the plight of another person, and feel like the other person. It means understanding things from the other person’s perspective, i.e. putting oneself in the other person’s shoes. Empathy enriches the therapeutic relationship and transforms it into a healing relationship.
- The therapeutic alliance requires that the therapist must keep strict confidentiality of the experiences, events, feelings or thoughts disclosed by the client.
- The therapist must not exploit the trust and the confidence of the client in anyway.
- It must remain a professional relationship.
Type of Therapies
- Books Name
- Psychology Book Class-12
- Publication
- PathSet Publications
- Course
- CBSE Class 12
- Subject
- Psychology
Type of Therapies
Psychotherapies differ greatly in concepts, methods, and techniques.
The classification of psychotherapies into psychodynamic, behaviour, and existential is based on the following parameters:
- What is the cause, which has led to the problem?
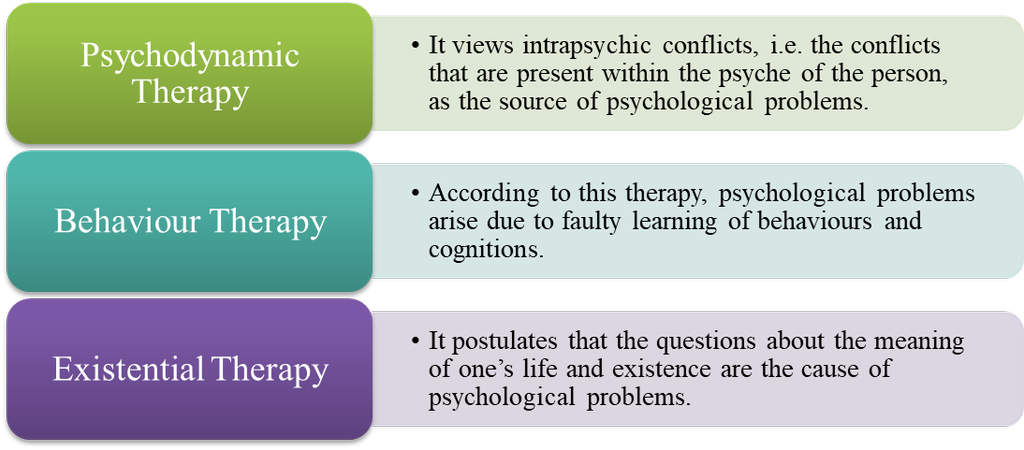
- How did the cause come into existence?
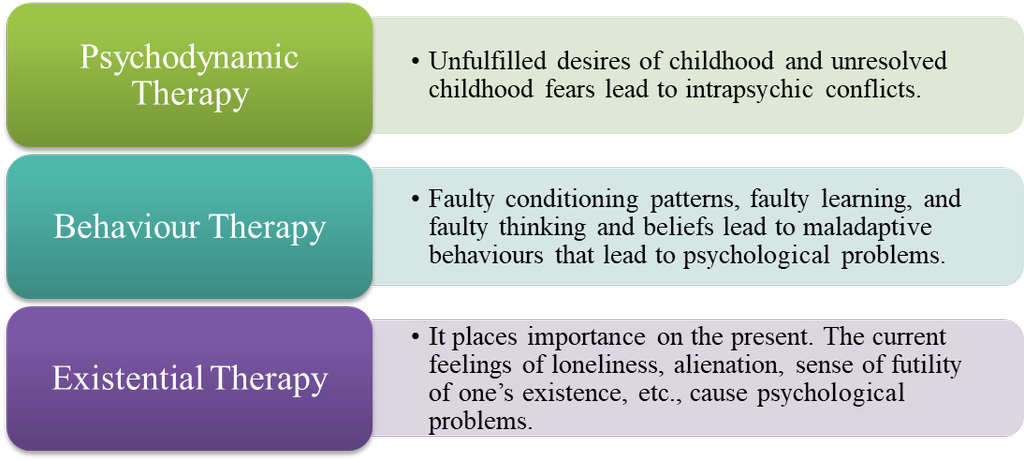
- What is the chief method of treatment?
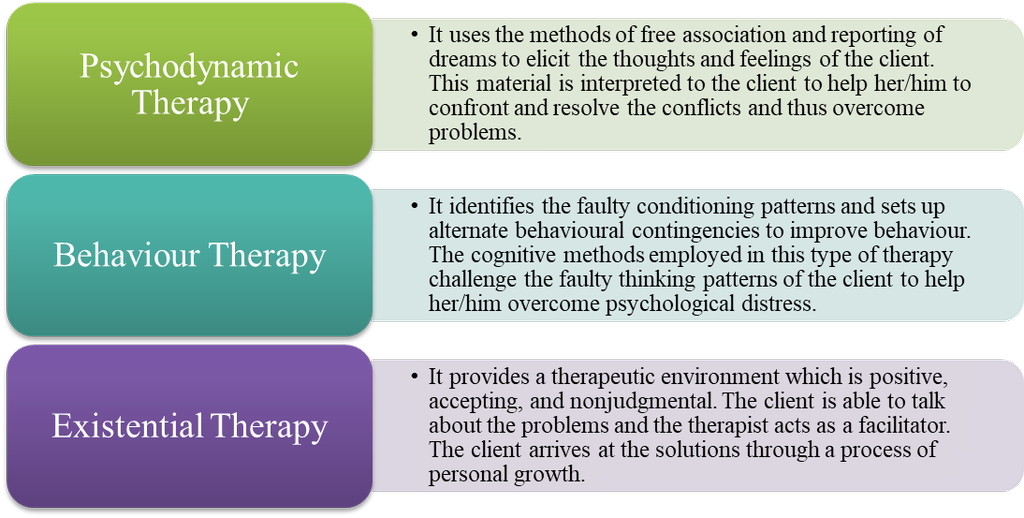
- What is the nature of therapeutic relationship between a client and therapist?
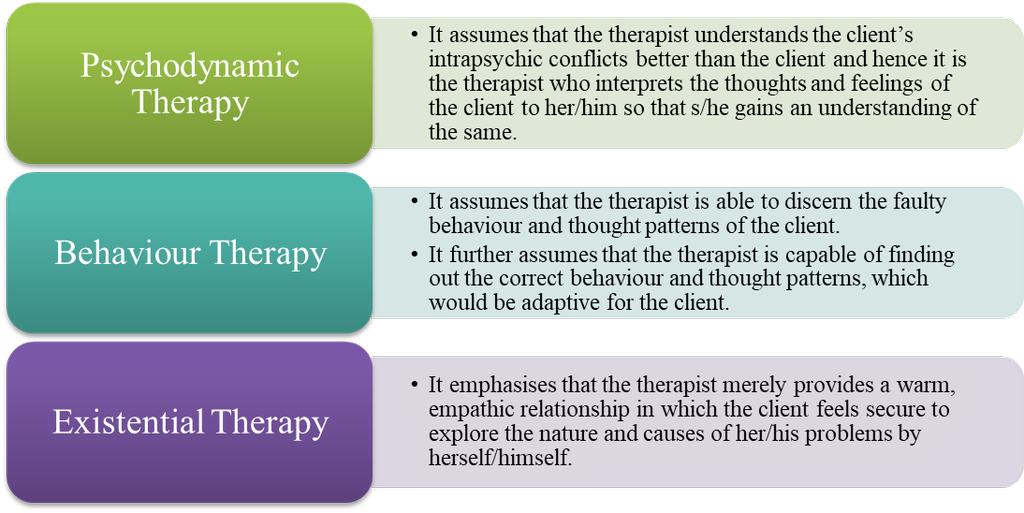
Both the psychodynamic and the behaviour therapies assume that the therapist is capable of arriving at solutions to the client’s problems, in contrast to existential therapy.
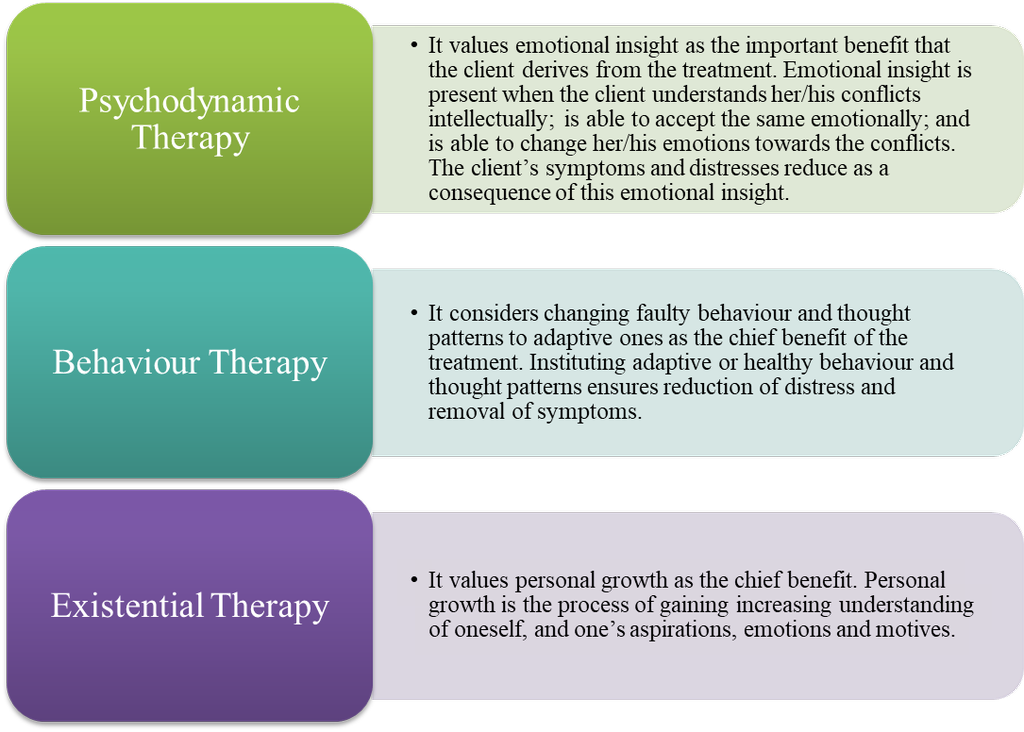
- What is the chief benefit to the client?
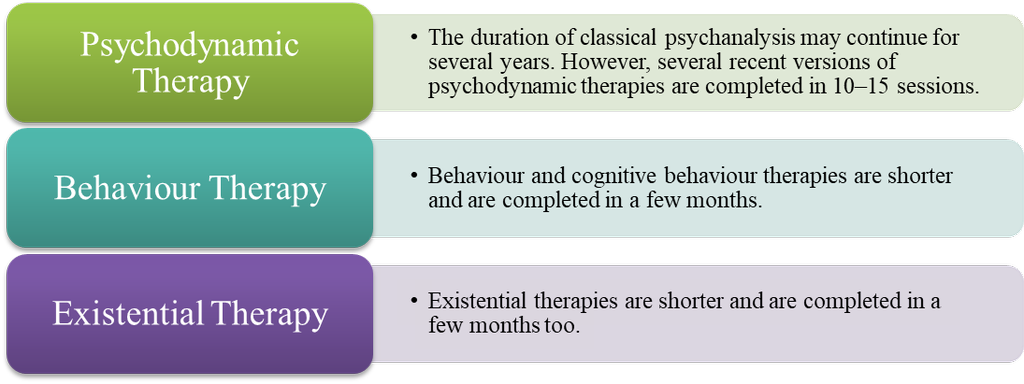
- What is the duration of treatment
Psychotherapy
- Books Name
- Psychology Book Class-12
- Publication
- PathSet Publications
- Course
- CBSE Class 12
- Subject
- Psychology
Psychodynamic Therapy (pioneered by Sigmund Freud)
- Carl Jung’s modified version of psychodynamic therapy is the analytical psychotherapy.
- Broadly, the psychodynamic therapy has conceptualised the structure of the psyche, dynamics between different components of the psyche, and the source of psychological distress.
- Methods of Eliciting the Nature of Intrapsychic Conflict
Since the psychoanalytic approach views intrapsychic conflicts to be the cause of psychological disorder, the first step in the treatment is to elicit this intrapsychic conflict.
Psychoanalysis has invented two important methods for eliciting the intrapsychic conflicts:
- The Free Association Method
- Main method for understanding the client’s problems.
- Once a therapeutic relationship is established, and the client feels comfortable, the therapist makes her/him lie down on the couch, close her/his eyes and asks her/ him to speak whatever comes to mind without censoring it in anyway.
- The client is encouraged to freely associate one thought with another, and this method is called the method of free association.
- The censoring superego and the watchful ego are kept in abeyance as the client speaks whatever comes to mind in an atmosphere that is relaxed and trusting.
- As the therapist does not interrupt, the free flow of ideas, desires and conflicts of the unconscious, which had been suppressed by the ego, emerge into the conscious mind.
- This free uncensored verbal narrative of the client is a window into the client’s unconscious to which the therapist gains access.
- Dream Interpretation
- The client is asked to write down her/his dreams upon waking up.
- Psychoanalysts look upon dreams as symbols of the unfulfilled desires present in the unconscious.
- The images of the dreams are symbols which signify intrapsychic forces.
- Dreams use symbols because they are indirect expressions and hence would not alert the ego.
- If the unfulfilled desires are expressed directly, the ever-vigilant ego would suppress them and that would lead to anxiety.
- These symbols are interpreted according to an accepted convention of translation as the indicators of unfulfilled desires and conflicts.
Modality of Treatment (Transference and Interpretation are the means of treating the patient)
- Transference
- As the unconscious forces are brought into the conscious realm through free association and dream interpretation, the client starts identifying the therapist with the authority figures of the past, usually childhood.
- The therapist may be seen as the punitive father, or as the negligent mother.
- The therapist maintains a non-judgmental yet permissive attitude and allows the client to continue with this process of emotional identification. This is the process of transference.
- The therapist encourages this process because it helps her/him in understanding the unconscious conflicts of the client.
- The client acts out her/his frustrations, anger, fear, and depression that s/he harboured towards that person in the past, but could not express at that time.
- The therapist becomes a substitute for that person in the present. This stage is called transference neurosis.
- A full-blown transference neurosis is helpful in making the therapist aware of the nature of intrapsychic conflicts suffered by the client.
- There is the positive transference in which the client idolises, or falls in love with the therapist, and seeks the therapist’s approval.
- Negative transference is present when the client has feelings of hostility, anger, and resentment towards the therapist.
- Resistance
- The process of transference is met with resistance.
- Since the process of transference exposes the unconscious wishes and conflicts, thereby increasing the distress levels, the client resists transference.
- Due to resistance, the client opposes the progress of therapy in order to protect herself/himself from the recall of painful unconscious memories.
- Resistance can be:
- Conscious
- the client deliberately hides some information
- Unconscious
- the client becomes silent during the therapy session
- the client recalls trivial details without recalling the emotional ones
- the client misses appointments
- the client comes late for therapy sessions.
- The therapist overcomes the resistance by repeatedly confronting the patient about it and by uncovering emotions such as anxiety, fear, or shame, which are causing the resistance.
- Interpretation
- Fundamental mechanism by which change is effected.
- Two analytical techniques of interpretation are:
- In confrontation, the therapist points out to the client an aspect of her/his psyche that must be faced by the client.
- Clarification is the process by which the therapist brings a vague or confusing event into sharp focus. This is done by separating and highlighting important details about the event from unimportant ones.
- A more subtle process.
- Considered to be the pinnacle of psychoanalysis.
- The therapist uses the unconscious material that has been uncovered in the process of free association, dream interpretation, transference and resistance to make the client aware of the psychic contents and conflicts which have led to the occurrence of certain events, symptoms and conflicts.
- Interpretation can focus on intrapsychic conflicts or on deprivations suffered in childhood.
- Working Through
- The repeated process of using confrontation, clarification, and interpretation.
- Helps the patient to understand herself/himself and the source of the problem and to integrate the uncovered material into her/his ego.
- Insight
- The outcome of working through is insight.
- A gradual process wherein the unconscious memories are repeatedly integrated into conscious awareness; these unconscious events and memories are re-experienced in transference and are worked through.
- As this process continues, the client starts to:
- understand herself/himself better at an intellectual and emotional level
- gain insight into her/his conflicts and problems
- The intellectual understanding is the intellectual insight.
- The emotional insight is:
- emotional understanding
- acceptance of one’s irrational reaction to the unpleasant events of the past
- willingness to change emotionally as well as making the change
- Insight is the end point of therapy as the client has gained a new understanding of herself/himself.
- The client becomes a psychologically healthy person as the conflicts of the past, defence mechanisms and physical symptoms are no longer present.
- Psychoanalysis is terminated at this stage.
Duration of Treatment
- Psychoanalysis lasts for several years, with 1 hour session for 4–5 days per week.
- It is an intense treatment.
- There are three stages in the treatment:
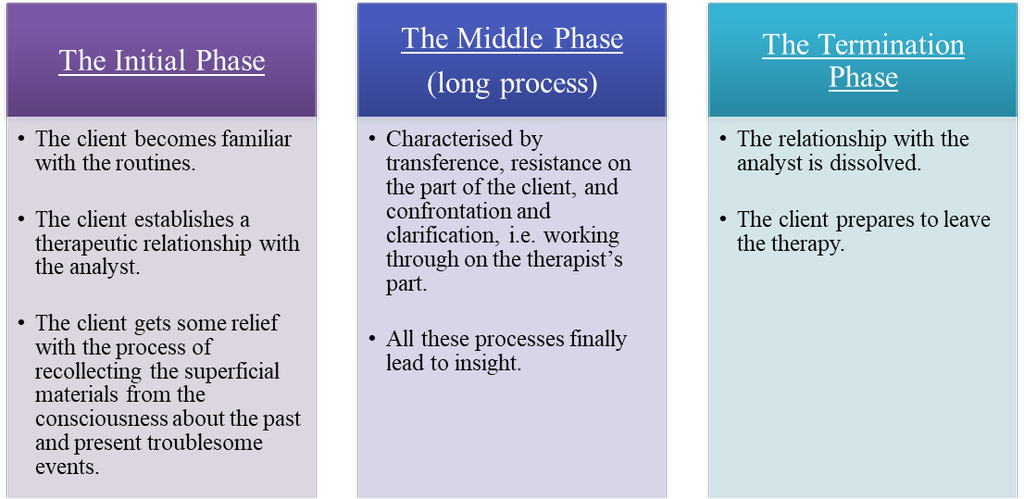
Behaviour Therapy
- It postulate that psychological distress arises because of faulty behaviour patterns or thought patterns.
- Focused on the behaviour and thoughts of the client in the present. The past is relevant only to the extent of understanding the origins of the faulty behaviour and thought patterns. The past is not activated or relived.
- The clinical application of learning theory principles constitute behaviour therapy.
- The symptoms of the client and the clinical diagnosis are the guiding factors in the selection of the specific techniques or interventions to be applied, therefore it is not a unified theory.
- For example,
- Treatment of phobias or excessive and crippling fears would require the use of one set of techniques while that of anger outbursts would require another.
- A depressed client would be treated differently from a client who is anxious.
- The foundation of behaviour therapy is on formulating dysfunctional or faulty behaviours, the factors which reinforce and maintain these behaviours, and devising methods by which they can be changed.
Method of Treatment
- The client with psychological distress or with physical symptoms, which cannot be attributed to physical disease, is interviewed with a view to analyse her/his behaviour patterns.
- Behavioural analysis is conducted to find:
Malfunctioning behaviours
Malfunctioning behaviours are those behaviours which cause distress to the client.
Antecedents of faulty learning
Antecedent factors are those causes which predispose the person to indulge in that behaviour.
Factors that maintain or continue faulty learning
Maintaining factors are those factors which lead to the persistence of the faulty behaviour.
- Once the faulty behaviours which cause distress, have been identified, a treatment package is chosen.
- The aim of the treatment is to extinguish or eliminate the faulty behaviours and substitute them with adaptive behaviour patterns.
- The therapist does this through establishing antecedent operations and consequent operations. Antecedent operations control behaviour by changing something that precedes such a behaviour. The change can be done by increasing or decreasing the reinforcing value of a particular consequence. This is called establishing operation.
Behavioural Techniques
- The principles of these techniques are to:
- reduce the arousal level of the client
- alter behaviour through classical conditioning or operant conditioning with different contingencies of reinforcements
- use vicarious learning procedures, if necessary.
- The skill of the therapist lies in conducting an accurate behavioural analysis and building a treatment package with the appropriate techniques.
- Negative reinforcement (major technique of behaviour modification)
- Responses that lead organisms to get rid of painful stimuli or avoid and escape from them provide negative reinforcement.
- One learns to move away from dangerous stimuli because they provide negative reinforcement. For example, one learns to put on woollen clothes, burn firewood or use electric heaters to avoid the unpleasant cold weather.
- Aversive conditioning (another major technique of behaviour modification)
- It refers to repeated association of undesired response with an aversive consequence.
- For example, an alcoholic is given a mild electric shock and asked to smell the alcohol. With repeated pairings the smell of alcohol is aversive as the pain of the shock is associated with it and the person will give up alcohol
- Positive reinforcement
- If an adaptive behaviour occurs rarely, positive reinforcement is given to increase the deficit.
- For example, if a child does not do homework regularly, positive reinforcement may be used by the child’s mother by preparing the child’s favourite dish whenever s/he does homework at the appointed time. The positive reinforcement of food will increase the behaviour of doing homework at the appointed time.
- Token economy
- Persons with behavioural problems can be given a token as a reward every time a wanted behaviour occurs. The tokens are collected and exchanged for a reward such as an outing for the patient or a treat for the child.
- Differential Reinforcement
- Unwanted behaviour can be reduced and wanted behaviour can be increased simultaneously through differential reinforcement.
- Positive reinforcement for the wanted behaviour and negative reinforcement for the unwanted behaviour attempted together may be one such method.
- The other method is to positively reinforce the wanted behaviour and ignore the unwanted behaviour. This method is less painful and equally effective.
- Systematic desensitisation
- It is a technique introduced by Wolpe for treating phobias or irrational fears.
- The client is interviewed to elicit fearprovoking situations and together with the client, the therapist prepares a hierarchy of anxiety-provoking stimuli with the least anxiety-provoking stimuli at the bottom of the hierarchy.
- The therapist relaxes the client and asks the client to think about the least anxiety-provoking situation.
- The client is asked to stop thinking of the fearful situation if the slightest tension is felt.
- Over sessions, the client is able to imagine more severe fearprovoking situations while maintaining the relaxation.
- The client gets systematically desensitised to the fear.
- The principle of reciprocal inhibition operates here, which states that the presence of two mutually opposing forces at the same time, inhibits the weaker force.
- Thus, the relaxation response is first built up and mildly anxiety-provoking scene is imagined, and the anxiety is overcome by the relaxation.
- The client is able to tolerate progressively greater levels of anxiety because of her/his relaxed state.
- Modelling
- It is the procedure wherein the client learns to behave in a certain way by observing the behaviour of a role model or the therapist who initially acts as the role model.
- Vicarious learning, i.e. learning by observing others, is used and through a process of rewarding small changes in the behaviour, the client gradually learns to acquire the behaviour of the model.
Cognitive Therapy
- It locates the cause of psychological distress in irrational thoughts and beliefs.
- Rational Emotive Therapy (RET) by Albert Ellis
- The central thesis of this therapy is that irrational beliefs mediate between the antecedent events and their consequences.
- The first step in RET is the antecedent-belief-consequence (ABC) analysis.
- Antecedent events, which caused the psychological distress, are noted.
- The client is also interviewed to find the irrational beliefs, which are distorting the present reality. Irrational beliefs may not be supported by empirical evidence in the environment. These beliefs are characterised by thoughts with ‘musts’ and ‘shoulds’, i.e. things ‘must’ and ‘should’ be in a particular manner.
Example “One should be loved by everybody all the time”
- This distorted perception of the antecedent event due to the irrational belief leads to the consequence, i.e. negative emotions and behaviours.
- Irrational beliefs are assessed through questionnaires and interviews.
- In the process of RET, the irrational beliefs are refuted by the therapist through a process of non-directive questioning. The nature of questioning is gentle, without probing or being directive.
- The questions make the client to think deeper into her/his assumptions about life and problems.
Gradually the client is able to change the irrational beliefs by making a change in her/his philosophy about life.
- The rational belief system replaces the irrational belief system and there is a reduction in psychological distress
- Aaron Beck’s Theory
- This theroy of psychological distress characterised by anxiety or depression, states that childhood experiences provided by the family and society develop core schemas or systems, which include beliefs and action patterns in the individual.
For example,
a client, who was neglected by the parents as a child, develops the core schema of “I am not wanted”. During the course of life, a critical incident occurs in her/his life. S/he is publicly ridiculed by the teacher in school. This critical incident triggers the core schema of “I am not wanted” leading to the development of negative automatic thoughts. Negative thoughts are persistent irrational thoughts such as “nobody loves me”, “I am ugly”, “I am stupid”, “I will not succeed”, etc. Such negative automatic thoughts are characterised by cognitive distortions.
Cognitive distortions are ways of thinking which are general in nature but which distort the reality in a negative manner.
These patterns of thought are called dysfunctional cognitive structures which lead to errors of cognition about the social reality.
- Repeated occurrence of these thoughts leads to the development of feelings of anxiety and depression.
- The therapist uses questioning, which is gentle, nonthreatening disputation of the client’s beliefs and thoughts.
Example “Why should everyone love you?”
- The questions make the client think in a direction opposite to that of the negative automatic thoughts whereby s/he gains insight into the nature of her/his dysfunctional schemas, and is able to alter her/his cognitive structures.
- The aim of the therapy is to achieve this cognitive restructuring which, in turn, reduces anxiety and depression.
- Similar to behaviour therapy, cognitive therapy focuses on solving a specific problem of the client. Behaviour therapy is open, i.e. the therapist shares her/his method with the client. It is short, lasting between 10–20 sessions.
- Cognitive Behaviour Therapy (CBT)
- Most popular therapy presently
- Short and efficacious treatment for a wide range of psychological disorders such as anxiety, depression, panic attacks, and borderline personality, etc.
- CBT adopts a bio-psychosocial approach to the delineation of psychopathology.
- It combines cognitive therapy with behavioural techniques.
- The rationale is that the client’s distress has its origins in the biological, psychological, and social realms. Hence, addressing:
- the biological aspects through relaxation procedures
- the psychological ones through behaviour and cognitive therapy techniques
- the social ones with environmental manipulations
- CBT is a comprehensive technique which is:
- easy to use
- applicable to a variety of disorders
- has proven efficacy
Humanistic-existential Therapy
- It postulates that psychological distress arises from feelings of:
- Loneliness
- Alienation
- An inability to find meaning and genuine fulfilment in life
- Human beings are motivated by the desire for personal growth and self-actualisation, and an innate need to grow emotionally.
When these needs are curbed by society and family, human beings experience psychological distress.
- Self-actualisation is defined as an innate or inborn force that moves the person to become more complex, balanced, and integrated, i.e. achieving the complexity and balance without being fragmented.
- Integrated means a sense of whole, being a complete person, being in essence the same person in spite of the variety of experiences that one is subjected to.
- Healing occurs when the client is able to perceive the obstacles to self-actualisation in her/his life and is able to remove them.
- Self-actualisation requires free emotional expression which gets curbed by the family and society as it is feared that a free expression of emotions can harm society by unleashing destructive forces.
This curb leads to destructive behaviour and negative emotions by thwarting the process of emotional integration.
- Therefore, the therapy creates a permissive, non-judgmental and accepting atmosphere in which the client’s emotions can be freely expressed and the complexity, balance and integration could be achieved.
- The fundamental assumption is that the client has the freedom and responsibility to control her/his own behaviour.
The therapist is merely a facilitator and guide. It is the client who is responsible for the success of therapy.
- The chief aim of the therapy is to expand the client’s awareness.
- Healing takes place by a process of understanding the unique personal experience of the client by herself/himself.
- The client initiates the process of self-growth through which healing takes place.
- Existential Therapy
- Victor Frankl, a psychiatrist and neurologist propounded the Logotherapy.
- Logos is the Greek word for soul and Logotherapy means treatment for the soul.
- Frankl calls this process of finding meaning even in life-threatening circumstances as the process of meaning making.
- The basis of meaning making is a person’s quest for finding the spiritual truth of one’s existence.
- There is a spiritual unconscious, which is the storehouse of:
- Love
- Aesthetic awareness
- Values of life
- Neurotic anxieties arise when the problems of life are attached to the physical, psychological or spiritual aspects of one’s existence.
- He emphasised the role of spiritual anxieties in leading to meaninglessness and hence it may be called an existential anxiety, i.e. neurotic anxiety of spiritual origin.
- The goal of logotherapy is to help the patients to find meaning and responsibility in their life irrespective of their life circumstances.
- The therapist:
- emphasises the unique nature of the patient’s life
- encourages them to find meaning in their life
- is open and shares her/his feelings, values and his/her own existence with the client
- reminds the client about the immediacy of the present
- The emphasis is on here and now.
- Transference is actively discouraged.
- The goal is to facilitate the client to find the meaning of her/his being.
- Client-centred Therapy by Carl Rogers
- Rogers combined scientific rigour with the individualised practice of client-centred psychotherapy.
- He brought into psychotherapy the concept of self, with freedom and choice as the core of one’s being.
- The therapy provides a warm relationship in which the client can reconnect with her/his disintegrated feelings.
- The therapist shows empathy, i.e. understanding the client’s experience as if it were her/his own, is warm and has unconditional positive regard, i.e. total acceptance of the client as s/he is.
- Empathy sets up an emotional resonance between the therapist and the client.
- Unconditional positive regard indicates that the positive warmth of the therapist is not dependent on what the client reveals or does in the therapy sessions.
- This unique unconditional warmth ensures that the client feels secure and can trust the therapist. The client feels secure enough to explore her/his feelings.
- The therapist reflects the feelings of the client in a non-judgmental manner. The reflection is achieved by rephrasing the statements of the client, i.e. seeking simple clarifications to enhance the meaning of the client’s statements.
- This process of reflection helps the client to become integrated.
- Personal relationships improve with an increase in adjustment.
- In essence, this therapy helps a client to become her/his real self with the therapist working as a facilitator.
- Gestalt Therapy by Freiderick (Fritz) Perls and Laura Perls
- The German word gestalt means ‘whole’.
- The goal is to increase an individual’s self-awareness and self-acceptance.
- The client is taught to recognise the bodily processes and the emotions that are being blocked out from awareness.
- The therapist does this by encouraging the client to act out fantasies about feelings and conflicts.
Biomedical Therapy
- Medicines
- They may be prescribed to treat psychological disorders but only by qualified medical professionals known as psychiatrists who are medical doctors who have specialised in the understanding, diagnosis and treatment of mental disorders.
- The nature of medicines used depends on the nature of the disorders.
For examples,
- Severe mental disorders such as schizophrenia or bipolar disorder require anti-psychotic drugs.
- Common mental disorders such as generalised anxiety or reactive depression may also require milder drugs.
- The medicines prescribed to treat mental disorders can cause side-effects which need to be understood and monitored. Hence, it is essential that medication is given under proper medical supervision.
- Those drugs which normal individuals use to stay awake to study for examinations or to get a ‘high’ at a party have dangerous side-effects as they can cause:
- Addiction
- Harm to the brain and the body.
Therefore, it is dangerous to self-medicate with drugs which affect the mind.
- Electro-convulsive Therapy (ECT)
- It is another form of biomedical therapy.
- Mild electric shock is given via electrodes to the brain of the patient to induce convulsions.
- The shock is given by the psychiatrist only when it is necessary for the improvement of the patient.
- ECT is not a routine treatment
- It is given only when drugs are not effective in controlling the symptoms of the patient.
Alternative Therapies
- They are alternative treatment possibilities to the conventional drug treatment or psychotherapy.
- There are many alternative therapies such as:
- Yoga
- Meditation
- Acupuncture
- Herbal remedies
- In the past 25 years, yoga and meditation have gained popularity as treatment programmes for psychological distress.
- Yoga
- an ancient Indian technique detailed in the Ashtanga Yoga of Patanjali’s Yoga Sutras
- refers to:
- asanas (body posture component), or
- breathing practices (pranayama), or
- combination of the two
- Meditation
- practice of focusing attention on breath or on an object or thought or a mantra
- here attention is focused.
- Vipasana meditation (mindfulness-based meditation)
- there is no fixed object or thought to hold the attention
- person passively observes the various bodily sensations and thoughts that are passing through in her or his awareness.
- help the patients to process emotional stimuli better and hence prevent biases in the processing of these stimuli
- help with prevention of repeated episodes of depression
- Sudarshana Kriya Yoga (SKY)
- Involves the rapid breathing techniques to induce hyperventilation
- Beneficial, low-risk, low-cost adjunct to the treatment of stress, anxiety, post-traumatic stress disorder (PTSD), depression, stressrelated medical illnesses, substance abuse, and rehabilitation of criminal offenders.
- Has been used as a public health intervention technique to alleviate PTSD in survivors of mass disasters.
- Reduces depression (shown by Research conducted at the National Institute of Mental Health and Neurosciences (NIMHANS))
- Alcoholic patients who practice SKY have reduced depression and stress levels.
- Yoga techniques enhance
- well-being
- mood
- attention
- mental focus
- stress tolerance
- Yoga reduces the time to go to sleep and improves the quality of sleep, hence helping with treatment of insomnia.
- Proper training by a skilled teacher and a 30-minute practice every day will maximise the benefits.
- Kundalini Yoga (taught in the USA)
- Effective in treatment of mental disorders
- Effective in the treatment of obsessive-compulsive disorder (found by The Institute for Nonlinear Science, University of California, San Diego, USA)
- Combines pranayama (breathing techniques) with chanting of mantras.
Factors Contributing to Healing in Psychotherapy
- Major factor in the healing is the techniques adopted by the therapist and the implementation of the same with the patient/client.
For instance, if the behavioural system and the CBT school are adopted to heal an anxious client, the relaxation procedures and the cognitive restructuring largely contribute to the healing.
- The therapeutic alliance, which is formed between the therapist and the patient/client, has healing properties, because of:
- the regular availability of the therapist
- the warmth and empathy provided by the therapist.
- The process of emotional unburdening which is known as ‘catharsis’ has healing properties.
At the outset of therapy while the patient/client is being interviewed in the initial sessions to understand the nature of the problem, s/he unburdens the emotional problems being faced.
- There are several non-specific factors associated with psychotherapy. These factors are called non-specific because they occur across different systems of psychotherapy and across different clients/patients and different therapists.
- Non-specific factors attributable to the client/patient are called patient vairables which include:
- motivation for change
- expectation of improvement due to the treatment
- Non-specific factors attributable to the therapist are called therapist variables which include:
- positive nature
- absence of unresolved emotional conflicts
- presence of good mental health
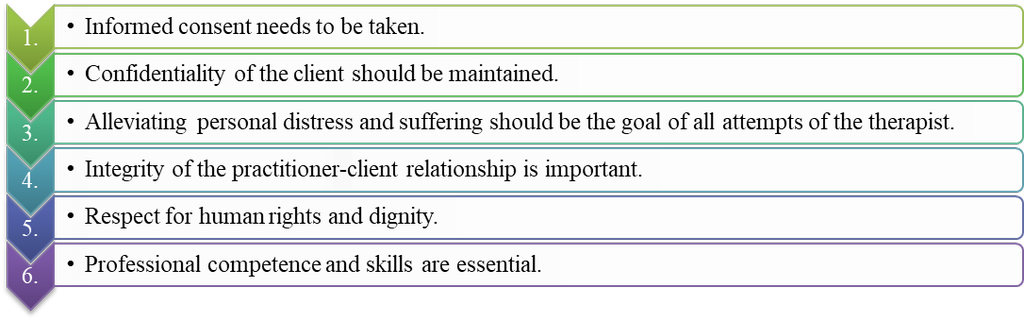
Ethics in Psychotherapy
Rehabilitation of the Mentally Ill
- Books Name
- Psychology Book Class-12
- Publication
- PathSet Publications
- Course
- CBSE Class 12
- Subject
- Psychology
Rehabilitation of the Mentally Ill
- The treatment of psychological disorders has two components
- reduction of symptoms
- improving the level of functioning or quality of life.
In the case of milder disorders (generalised anxiety, reactive depression or phobia) reduction of symptoms is associated with an improvement in the quality of life.
In the case of severe mental disorders (schizophrenia) reduction of symptoms may not be associated with an improvement in the quality of life.
- Many patients suffer from negative symptoms such as disinterest and lack of motivation to do work or to interact with people.
- Rehabilitation is required to help such patients become self-sufficient.
The aim of rehabilitation is to empower the patient to become a productive member of society to the extent possible.
- In rehabilitation, the patients are given:
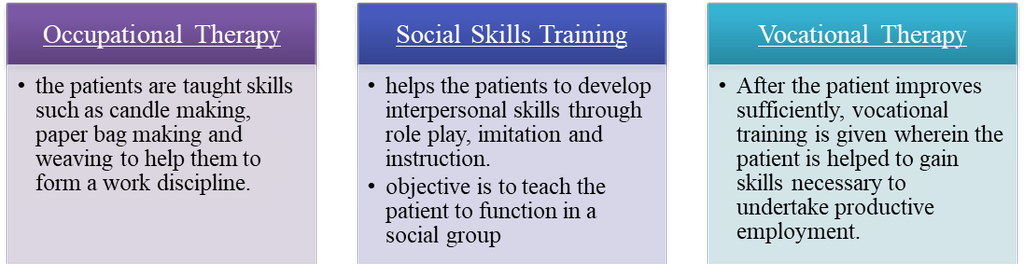
 PathSet Publications
PathSet Publications
