Indian Systems of Medicine (ISM)
- India has its own well-developed alternate system of health care, namely: AYUSH, consisting of six systems - Ayurveda, Yoga, Unani, Siddha, Naturopathy and Homeopathy.
- At present, there are 3,167 ISM hospitals, 26,000 dispensaries and as many as 7 lakh registered practitioners in India.
- ISM has huge potential and can solve a large part of our health ca. are effective, safe and inexpensive.
- However, little effort has been done to set up a framework to standardize education or promote research.
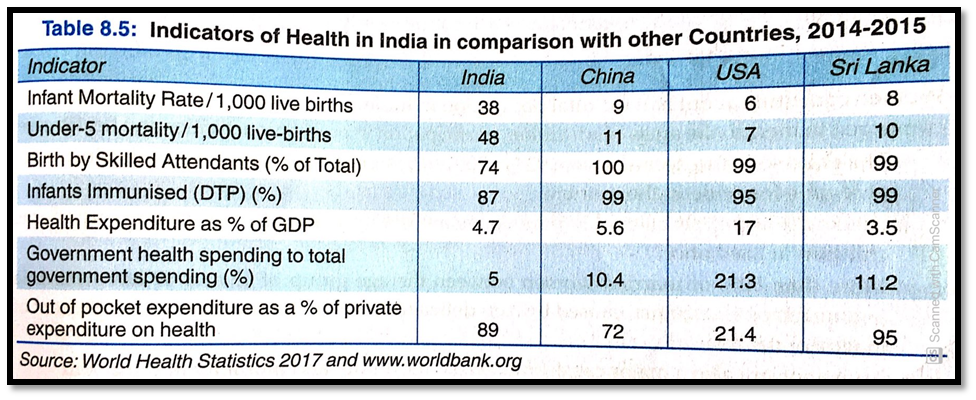
Indicators of Health and Health Infrastructure
- Expenditure on the health sector is just 4.7% of total GDP. It is extremely low as con d to other developed and developing countries.
- India has about 17% of the world's population but it bears a frightening 20% of the Global burden of diseases (GBD).
- Every year, around 5 lakh children die of water-borne diseases. The danger of AIDS is also looming large.
- Malnutrition and inadequate supply of vaccines lead to the death of 2.2 million children every year.
- At present, less than 20% of the population utilizes public health facilities and only 38% of the PHCs have the required number of doctors and only 30% of the PHCs have sufficient stock of medicines.
Rural-Urban Divide (Poor-Rich Divide)
- 70% of India's population live in rural areas, but only 20% of total hospitals and 500 total dispensaries are located in rural areas. Out of about 6.3 lakh beds in government hospitals, only 30% of beds are available in rural areas.
- There are only 0.36 hospitals for every one lakh people in rural areas, while urban are have 3.6 hospitals for the same number of people.
- The PHCs located in rural areas do not even offer X-ray or blood testing facilities, which constitutes basic healthcare. States like Bihar, Madhya Pradesh, Rajasthan and Uttar Pradesh are relatively lagging behind in health care facilities.
- In the rural areas, the percentage of people, who have no access to proper healthcare facilities, has increased over the last few years.
- Villagers have no access to any specialized medical care, like pediatrics, gynecology, anesthesia and obstetrics.
- Even though 380 recognized medical colleges produce 44,000 medical graduates every year, the shortage of doctors in rural areas persists. 20% of these graduates leave the country for better monetary prospects and many opt for private hospitals, located in the urban areas.
- The poorest 20% of Indians living in both urban and rural areas spend 12% of their income on healthcare while the rich spend only 2%.
Women Health
- Women constitute about half the total population in India. They suffer many disadvantages as compared to men, in the areas of education, participation in economic activities and health care.
- The child sex ratio declined from 927 in 2001 to 914 in 2011. It indicates a growing incidence of female foeticide in the country.
- Around 3 lakh girls below 15 years of age are not only married but have already borne children at least once.
- More than 50% of married women between the age group of 15 and 49 have anaemia and nutritional anaemia, caused by iron deficiency, which has contributed to 19% cent of maternal deaths.
- Abortions are also a major cause of maternal morbidity and mortality in India.
Health: A basic Human Right.
- All citizens can get better health facilities if public health services are decentralized.
- Success in the long-term battle against diseases depends on education and efficient health infrastructure. Therefore, it is important to create awareness of health and hygiene and provide efficient systems.
- Telecom and IT sectors can play an important role in improving the health process of the economy.
- The effectiveness of healthcare programs rests on primary healthcare. Therefore, serious steps should be taken to improve them.
- Private-Public Partnership (PPP) can effectively ensure reliability, quality and affordability of both drugs and medicare.
Critical assessment of Health Infrastructure
- Inequitable distribution of Health Services: The existing health system suffers from inequitable distribution of institutions and manpower. About 70% of India's population lives in rural areas, but only 20% of total hospitals are located in rural areas. Most modern health facilities are available only in urban areas.
- Communicable Diseases: Increasing attention is urgently needed for the prevention of Communicable diseases like AIDS (Acquired Immune Deficiency Syndrome), HIV (Human Immuno Deficiency Virus) and SARS (Severe Acute Respiratory Syndrome), through effective control measures.
- Poor Sanitation Facilities: Sanitation facilities are extremely poor in both rural and urban areas. About 30% of the houses in urban areas do not have toilet facilities and the condition in rural areas is even worse. Improvement in sanitation facilities is immediately needed for the good health of the people.
- Lack of Manpower: Even though India produces 12,000 medical graduates every year, still there is a huge shortage of manpower.
- Malnutrition: Widespread malnutrition poses a major threat to lives, especially in the case of children.
- Role of Private Sector: Public sector has not been so successful in providing adequate health structure. There is a need to increase the collaboration of the public sector with the private sector to meet the health care needs of people. The government should take serious steps to overcome these deficiencies, as improvement in the health status is necessary for increasing the productivity and growth of the economy.
 PathSet Publications
PathSet Publications
